- Visibility 132 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijos.2024.058
-
CrossMark
- Citation
Outcome of osteosynthesis and tensor fascia lata muscle pedicle bone graft in neglected femoral neck fracture in adults
- Author Details:
-
Dilip Kumar Pal
-
Animesh Kumar Singh *
-
Anshu Aryan
-
Pranay Kundu
Introduction
The management of displaced femoral neck fracture in young adult is still remains an unresolved riddle. Both the Non-union (NU) and Avascular Necrosis (AVN) are such a complication which needs to be addressed simultaneously. Even though, after emergent anatomical reduction and fixation many a times it progresses to AVN.[1] The incidence of AVN is 5.5 - 70% and that of non-union is 0 - 22% has been recorded in the literature.[2], [3], [4], [5] Head preserving surgery is the need of the time in young adults. Neglected femoral fracture in young adult is also not common due to lack of awareness, bias to get conservative treatment, avoiding surgical treatment, anaesthetic unfitness, illiteracy, low socio economic status etc.
Among the head preserving surgeries, Muscle Pedicle Bone Graft (MPBG) described by Meyer’s and Bakshi’s procedure are very popular. Where Meyer’s procedure used Quadriceps Femoris MPBG[6] and Bakshi’s used Tensor Fascia Lata (TFL) MPBG[7] for AVN, we have fixed the neglected fracture neck of femur in young patients by CRIF method and then TFL MPBG was fixed at the sub capital region of head with the help of a screw, to increase the vascularity of the femoral head.
Materials and Methods
In this retrospective study we operated on 15 young (age >18-50 years) patients with neglected (>3 week old) traumatic fracture neck of femur (garden stageIII and IV) were included while Patients age <18 yrs, >50 yrs, < 3week oldfracture, garden stage I & II, non-traumatic, pathological fracture were excluded.
All were treated first by doing MRI, then surface traction and adductor tenotomy was done in all cases. Then by CRIF with 6.5 CCS femoral head was fixed. Then by modifying the Baksi’s procedure by transfixing TFL MPBG with the 3.5 cortical screw in a slot at the sub capital region of the neck of femur, using light bulb technique so as to prevent dislodgement of the graft.
Post-operatively all the patients were allowed to sit on the bed as soon as pain was tolerable and were kept in the derotation boot plaster for 3 weeks after that non weight bearing crutch walking was started between 3 to 6 weeks and then gradual partial to full weight bearing was started between 6 to 12 weeks post operatively. All the patients were evaluated radiographically and clinically using modified Harris hip score at 3 months, 6 months, 12 months and 2 years respectively.
Surgical procedure
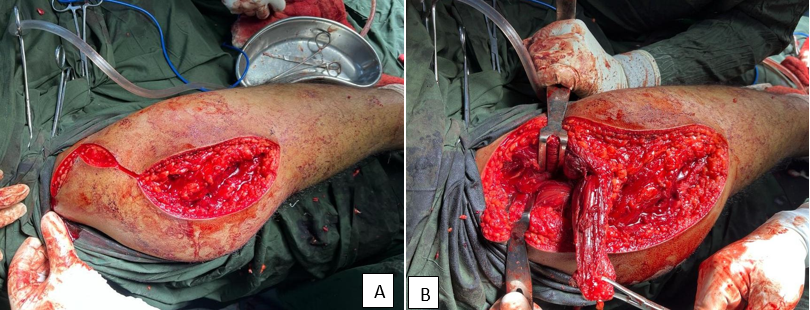
On the fracture table in the supine position the fracture neck of femur was reduced by the Lead Better manoeuvre.[8] Reduction was stabilised using 2-3 partially threaded 6.5 mm CCS. Then the hip was exposed using anterior Smith Peterson approach,[9] taking care of lateral cutaneous nerve of thigh. Then TFL MPBG was harvested from the ipsilateral iliac crest. About 2 cm x 2 cm of bone was excised with the help of oscillating saw, with the TFL attached over it. About 3cm thick central superficial muscular part of TFL was dissected up to the level of lesser trochanter.
|
Clinical details |
No. of cases |
|
Sex |
|
|
Males |
11 |
|
Females |
04 |
|
Anatomic class |
|
|
Sub capital |
2 |
|
Trans cervical |
9 |
|
Basi cervical |
4 |
|
Garden’s class |
|
|
Stage I and II |
0 |
|
Stage III |
8 |
|
Stage IV |
7 |
Then the capsule over the anterior aspect of subcapital region was exposed and about 1.5 cm oval window was created using K wire and osteotome. The TFL MPBG was then en-routed and turn inferiorly beneath the straight head of rectus femoris. Then the iliac crest bone graft was tailored to fit in the slot created over the subcapital region of the head. The graft position was secured using 3.5 mm cortical screw using lag principle, as in light bulb procedure. The hip was closed in layers with a drain kept in situ.
|
Complications |
No. of cases |
|
Non Union |
0 |
|
Delayed Union |
7 |
|
Coxa Vara |
4 |
|
LCNT injury |
4 |
|
Transient |
3 |
|
Permanent |
1 |
|
Screw backing |
4 |
|
Shortning |
|
|
Nil |
6 |
|
<1cm |
5 |
|
>1cm |
4 |
|
AVN |
0 |
Results
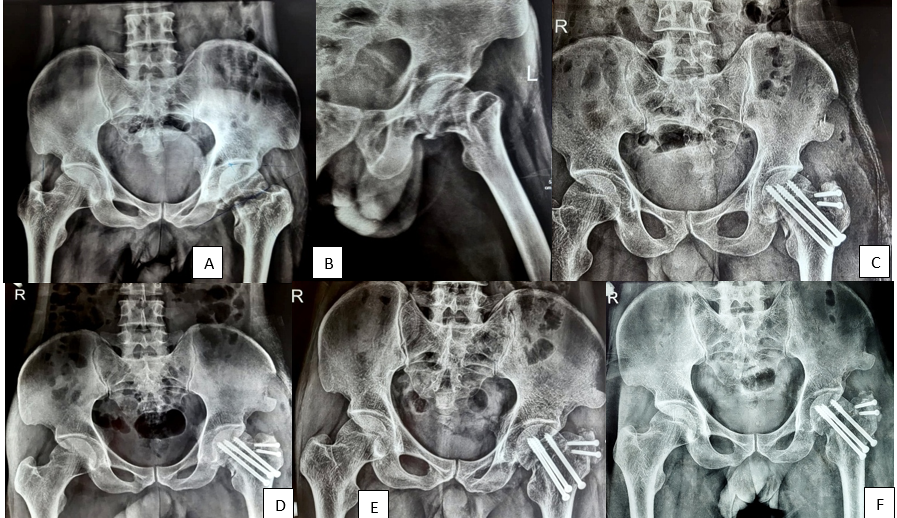
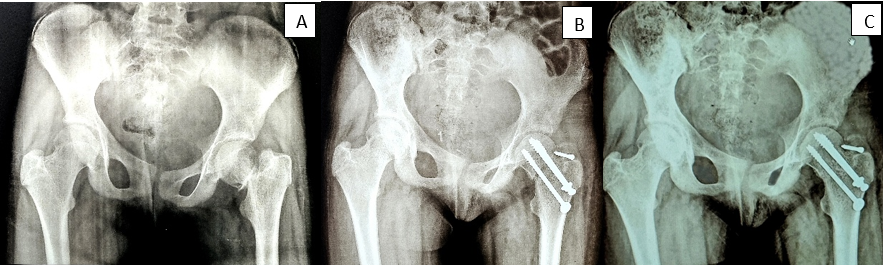
We operated on 18 patients of which 3 were lost to follow up and were excluded from the study. Of the remaining 15 patients, 11 were male and 4 were female. Average age of the patient was 27.8 years. 9 had fracture in right and 6 had fracture in left hip. Anatomically majority had trans cervical 9, basis cervical 4, and sub capital 2 fractures. 8 had Garden stage III and 7 had Garden stage IV neck fracture ([Table 1]). In majority mode of injury was RTA in 10, followed by fall from height in 5. Associated injury of pelvic rami was in 3 and calcaneal fracture was in 2 patients.
The mean operative time of surgery was 2 hours 35 minute. Lateral cutaneous nerve of thigh was injured in 4 patients (3 transient and one permanent). In 3 wound healing took a longer duration due to superficial infection, which responded to broad spectrum I.V antibiotics. Shortening of 1.5 to 2 cm (average 1.75 cm) was noted in 9 (60%) of the patients postoperatively. Mean delay in surgery was 4.7 weeks (3-6 weeks). Some amount of terminal flexion and abduction was restricted in most of the cases. Delayed union was noted in 7 cases. No cases of non-union and AVN were noted. Mild Varus collapse was found in 4 cases ([Table 2]).
|
Scores |
No. of cases |
|
Excellent 91-100 |
8 |
|
Good 81-90 |
4 |
|
Fair 71-80 |
2 |
|
Poor <70 |
1 |
|
Studies |
% Non- union |
% AVN |
|
Meyer’s |
10 |
5 |
|
Bakshi’s |
25 |
- |
|
Gupta et al |
10.35 |
6.89 |
|
Our study |
0 |
0 |

Clinically and radiographically the union and AVN was assessed up to 2 years post operatively (Fig 2A to 4D). The modified Harris Hip score was evaluated at each stage of follow up (i.e. 3 months, 6 months, 12 months and 2 years) and was found to be improving in subsequent follow up. The modified Harris hip score [10] at the final follow up was excellent in 8 hips, good in 4 hips, fair in 2 hips and poor in one hip ([Table 3]). The patient with fair score are doing well with the help of walking stick and do not want any further intervention. The patient with poor score was suggested THR but patient is reluctant due to economic constraints.
Discussion
Undoubtedly head preserving surgeries in neglected displaced neck femur fracture in young adults is the need of the time, especially in those part of the world where late presentation is not uncommon. The non-union and AVN can only be best addressed with the anatomic reduction, rigid fixation and revascularization surgeries in the form of muscle pedicle bone graft. Though there are various methods of reduction and rigid fixation, open reduction and internal fixation has been associated with more incidences of AVN.[2], [3], [4], [5] Closed reduction internal fixation with 6.5 mm CCS in 2 or 3 number provides the best union rate as in our study.
There are various methods to increase the vascularity of the femoral head using MPBG. More popular being Meyer’s Quadratus Femoris and Baksi’s Tensor Fascia Lata MPBG. Some have even tried with the Iliopsoas[11] and Sartorius[12] MPBG. There are similar studies where by Gupta etal.,[13] in 2008 showed similar results with open reduction internal fixation with Meyer’s technique and showed similar rate of union and AVN. In another study Chaudhary 2008 [14] by closed reduction and internal fixation and Meyer’s technique showed good union rate of and no AVN, similar to our study ([Table 4]).
It has been shown in the literature that the fate of AVN is set at the time of injury and urgent or delay in fixation has nothing to do with its progress to AVN.[15] To prevent further AVN we did closed reduction and internal fixation and only anterior capsulotomy was done to fix the TFL MPBG with a screw, to prevent graft dislodgement. Maurer et al., in a cadaveric study showed that 2 screws may be an acceptable fixation.[16] In our study union rate was significantly higher and there were no cases of AVN in any patients. Sud et al. reported 22% of non-union and 10% of AVN by closed reduction and internal fixation with CCS. Asif et al., have shown that long term result of bipolar is also not very satisfactory. Juha Partanen et al., concluded in their study that functional outcome of osteosynthesis is better but reoperation rate was higher compared to the hemiarthroplasty group.[17]
Conclusion
We conclude that this method of treating neglected displaced fracture neck of femur in young adults using closed reduction internal fixation with 6.5 CCS and TFL MPBG fixed with a screw is a simple effective, economic and reproducible method. Though, THA can be easily carried out in failed cases. The sample size being very small in our study, the similar study on larger group is required to reach to a definitive conclusion.
Ethical Approval
This study was conducted aftr taking approval from the institute Ethical approval committee with ref. no. MGM/IEC-102/2023.
Conflict of Interest
None.
Source of Funding
None.
References
- RS Garden. Reduction and fixation of the subcapital fractures of the femur. Orthop Clin North Am 1974. [Google Scholar]
- SM Tooke, KJ Favero. Femoral neck fractures in skeletally mature patients, fifty years old or less. J Bone Joint Surg Am 1985. [Google Scholar]
- SR Askin, RS Bryan. Femoral neck fractures in young adults. Clin Orthop Relat Res 1976. [Google Scholar]
- MF Swiontkowski, RA Winquist, ST Hansen. Fractures of the femoral neck in patients between the ages of twelve and forty nine years. J Bone Joint Surg Am 1984. [Google Scholar]
- N Sugano, K Masuhara, N Nakamura, T Ochi, A Hirooka, Y Hayami. MRI of early osteonecrosis of the femoral head after transcervical fracture. J Bone Joint Surg Br 1996. [Google Scholar]
- MH Meyers, JP Harvey, TM Moore. Treatment of displaced subcapital and transcervical fractures of the femoral neck by muscle pedicle bone graft and internal fixation: A preliminary report on one hundred and fifty cases. J Bone Joint Surg Am 1973. [Google Scholar]
- DP Baksi. Internal fixation of ununited femoral neck fractures combined with muscle pedicle bone grafting. J Bone Joint Surg Br 1986. [Google Scholar]
- GW Leadbetter. Closed reduction of fractures of the neck of the femur. J Bone Joint Surg Am 1938. [Google Scholar]
- MN Smith-Petersen. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am 1949. [Google Scholar]
- WH Harris. Traumatic arthritis of the hip after dislocation in acetabular fracture treatment by mold arthroplasty. J Bone Joint Surg Am 1969. [Google Scholar]
- B Day, SS Shim, G Leung. The iliopsoas muscle pedicle bone graft: An experimental study of femoral head vascularity after subcapital fractures and hip dislocations. Clin Orthop Relat Res 1984. [Google Scholar]
- L Zhou, J Tan, Y Li. Treating avascular necrosis of femoral head in young adult by grafting sartorius muscle iliac bone flap. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2007. [Google Scholar]
- Ak Gupta, S Rastogi, R Nath. Internal fixation and muscle pedicle bone grafting in femoral neck fractures. Indian J Orthop 2008. [Google Scholar]
- S Chaudhuri. Closed reduction, internal fixation with quadratus femoris muscle pedicle bone grafting in displaced femoral neck fracture. Indian J Orthop 2008. [Google Scholar]
- F Razik, AS Alexopoulos, B El-Osta, MJ Connolly, A Brown, S Hassan. Time to internal fixation of femoral neck fractures in patients under sixty years--does this matter in the development of osteonecrosis of femoral head?. Int Orthop 2012. [Google Scholar]
- SG Maurer, KE Wright, FJ Kummer, JD Zuckerman, KJ Koval. Two or three screws for fixation of femoral neck fractures?. Am J Orthop (Belle Mead NJ) 2003. [Google Scholar]
- J Partanen, P Jalovaara. Functional comparison between uncemented Austin-Moore hemiarthroplasty and osteosynthesis with three screws in displaced femoral neck fractures—a matched-pair study of 168 patients. Int Orthop 2004. [Google Scholar]
