- Visibility 16 Views
- Downloads 4 Downloads
- DOI 10.18231/j.ijos.2020.008
-
CrossMark
- Citation
Efficacy of dynamic condylar screw for the treatment of distal femoral fractures: a prospective study
- Author Details:
-
S V L Narasimba Reddy
-
K Srinivas Yadav
-
Ashwin Kasturi *
Introduction
The longest and the strongest bone in the human body is the femur. A fracture to this bone causes a lot of morbidity. Distal femoral fractures to the femur involves a break in the lower 9-15 cm of the femur length up to the articular surface of the knee.[2], [1] Although the incidence of the proximal femoral fractures are 10 times more than distal femoral fractures, they are fairly common.[3] 31% of the femoral fracturs disregarding the hip fractures are said to be distal femoral fractures.[4] The incidences are more common in males around the age of 30 and in elderly females. The causes could most probably be due to increase in road traffic accidents and work place injuries in males and osteoporosis in females.[5]
In only about 50% of the cases, the non-operative method of treatment is satisfactory while with surgical treatment, it is satisfactory in 70-80% of the patients.[5] Prior to 1970 most supracondylar fractures were treated non-operatively; however, angular deformities, knee joint incongruity, loss of knee motion, as well as complications of recumbency led to better methods of treatment.[10], [9], [8], [7], [6]
In the 1970s the AO principles and the use of angled blade plate revolutionised the treatment of these injuries.[12], [11] It is now recognised by most orthopaedic surgeons that distal femur fractures are best treated by surgical fixation. Many devices are available including Dynamic Condylar Screw, Angled Blade Plate, Locking Compression Plate, Condylar Blade Plate and I.M Nailing.[14], [13] Internal fixation provides better outcomes than closed methods and allows early mobilisation.[15] However, all these methods are difficult and cumbersome, not to mention, not very useful in osteoporotic bones.
DCS is one such implant which has stood the test of time. The implant is cost-effective, and procedure, relatively easy to perform and affords a rigid internal fixation.[19], [18], [17], [16] The aim of this study is to assess the functional and radiological outcomes after DCS in terms of fracture alignment, stability and Varus collapse in distal femur fractures
Materials and Methods
This prospective study was done by the Department of Orthopaedics at Malla Reddy institute of Medical Sciences, Suraram, Hyderabad, over a period of two years from March 2017 to march 2019 on 56 patients aged above 18 years with distal femur fractures.
Patients with grade 3 compound injuries and pathological fractures were excluded. Fractures were classified according to AO/OTA TYPE 33(A-C).
On admission, all the patients’ demographic details were noted and all were subjected to thorough clinical examination. Blood was collected and sent for Random blood sugar, complete blood picture, Erythrocyte sedimentation rate, Lipid Profile, viral markers.
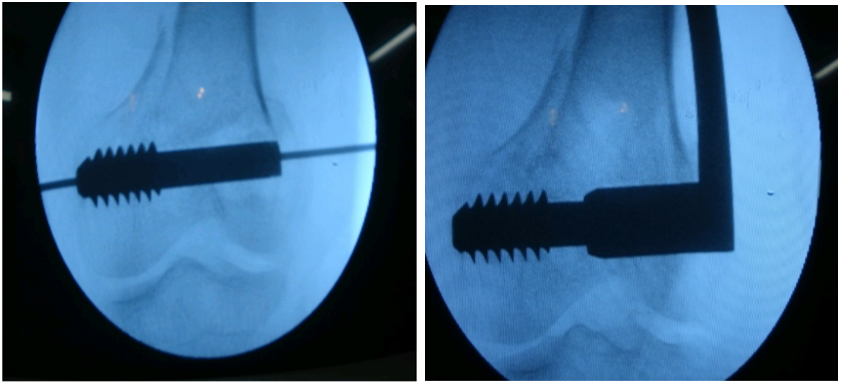
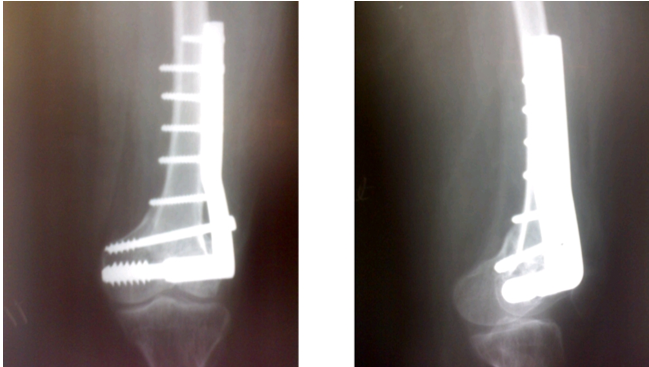
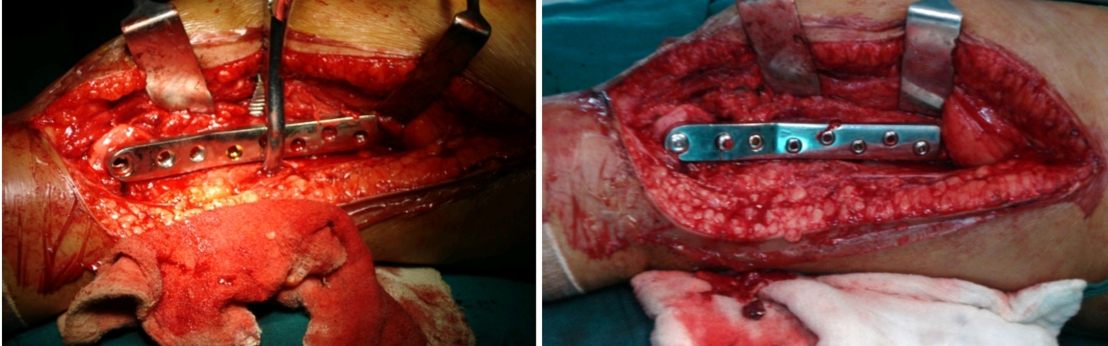
The patients were operated under spinal anaesthesia. A sand bag was used under the ipsilateral hemi pelvis. Lateral approach was used to expose the femur. Vastus lateralis was separated from lateral intermuscular septum and femur and retracted anteriorly. Guide wire was passed into the condyles parallel to the joint line under C-arm guidance. Lag screw was passed after reaming and tapping over the guide wire. Barrel plate was passed over the lag screw and fixed to shaft with cortical screws. Suction drain was used in all cases. Radiographs were taken on 1st POD. Change of dressing and drain removal was done on 2nd POD. Suture removal was done on 10th POD. Follow-up radiographs were taken at 6 weeks, 3 months and 6 months. Results were assessed using Knee Society Score.
Results
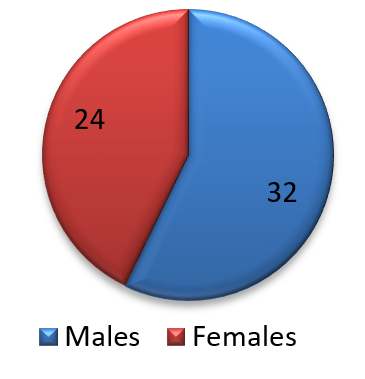
Out of the 56 patients in the study, there was a slight preponderance of males with 32 (57.14%) over females who were 24 (42.86%) in number ([Figure 1]).
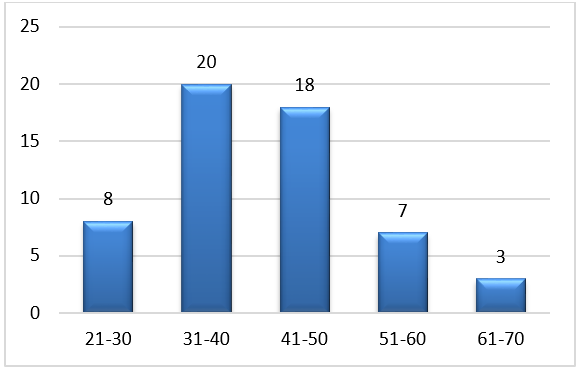
The predominant age group for the femoral fractures is 31-40 years (n=20, 35.7%) followed by 41-50 years n=18. 32.1%). 8 patients (14.3%) were between the ages 21-30 years and 7 (12.5%) were 51-60 years ([Figure 2]).
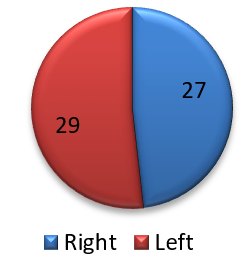
More than half of the patients had the fracture on the left side of the body (52%) and 27 of them (48%) had it on the right side. This difference however was not significant ([Figure 3]).
AO/OTA classification was used to classify the fractures. Type A fractures were seen in 43(76.78%), type B in 5(8.92%) and type C in 8(14.28%) of patients ([Table 1]). Out of 56 cases 6(10.71%) cases had open fractures, out of which 4 were grade 1, and 2 were grade 2 injuries ([Table 1]).
| Type | Number | Percentage |
| A1 | 24 | 42.9% |
| A2 | 16 | 28.6% |
| A3 | 3 | 5.4% |
| B1 | 5 | 8.9% |
| B2 | 0 | 0 |
| B3 | 0 | 0 |
| C1 | 4 | 7.1% |
| C2 | 2 | 3.6% |
| C3 | 2 | 3.6% |
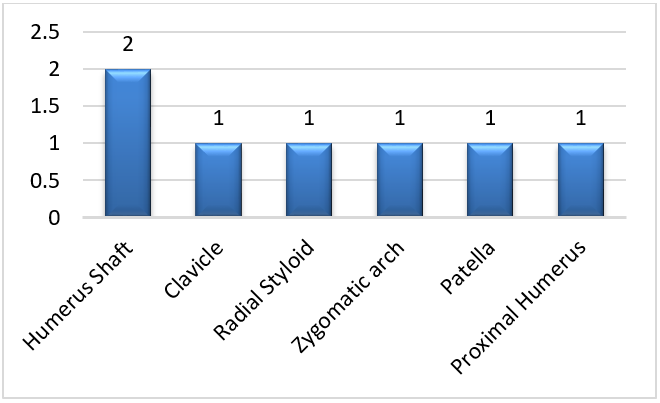
11(19.64%) of the patients had associated fractures. 4(7.14%) patients had colle’s fractures, 2(3.57%) had humerus shaft fractures. Clavicle fracture, radial styloid fracture, zygomatic arch fracture, proximal humerus fracture and patella fracture were seen in 1(1.78%) patient each ([Figure 4]).
The mechanical Lateral Distal Femoral Angle (mLDFA) was used to assess any post-operative varus collapse. The average mLDFA changed from 85o immediate post-op to 89o 6 months post-op. One patient with type C3 fracture had change of mLDFA from 87o to 95o. No statistically significant varus collapse was seen in our series. Two patients had post-operative wound infection, one which was superficial and subsided with antibiotics and dressings. The other was deeper and needed a reopening and wound wash. One patient had non-union which was treated with LCP and bone grafting. The average time to union in our study was 16 weeks.

Overall results were assessed using Knee Society Score. 31(55.36%) patients had excellent results, 14(25%) had good, 9(16.07%) had fair and 2(3.57%) had poor outcomes ([Table 2]).
| Result | Number | Percentage |
| Excellent | 31 | 55.36% |
| Good | 14 | 25% |
| Fair | 9 | 16.07% |
| Poor | 2 | 3.57% |
Discussion
High speed road traffic accidents are seen mostly in males of the younger age while a fall is the cause of femoral fracture in the elderly especially women, osteoporosis being the main cause.[20] The distal femoral fractures are most of the time multi-fragmentary and intraarticular, involving muscular forces, which makes the non-operative treatment very difficult. Decreased range of motion, pain and reduced function of knee usually is the cause of the failure of this treatment.[21]
Many techniques and implants have been tried for the treatment of such a fracture such as the ABP, CBP, cancellous screws, LCP, retrograde interlocking nail and DCS. For a few years now, DCS and LCP are the preferred surgeries performed for the treatment of these fractures.
In our study, males between 20-40 years and elderly females above 50 years were the chiefly affected persons. This was corroborated by a study by Chander et al, who also reported that males in their 20s were more likely to have fractures due to their involvement in road traffic accidents.[22] Another study by Reddy et al also reported road traffic accidents in young males and fall in elderly females to be the most common cause. [23]
Dunlop et al in their series of 31 fractures fixed with retrograde nailing had a mean age of 82. Type A fractures were 25 and type C were 6. Using neer’s score excellent were seen in 85%, satisfactory in 7.5% and unsatisfactory in 7.5%.[24] In the present study, the mean age was around 38.9 years, more because the males in the 20-40 age group were predominant in the study. We had 43 type A, 5 type B, and 8 type C fractures. Using Knee Society Score 55.6% of the patients had excellent results, and 25% had good results. Ostrum et al in their series of 30 patients, with a mean age of 48 years had 10 type A and 20 type C fractures. Using schatzker’s score 84% had good and excellent results, 111% had fair and 5% had poor outcomes.[25] Paknikar KP et al in their series of 50 patients with a mean age of 37.8 years had 8 type A, 1 type B and 41 type C fractures. Using Knee Society Score 32% had excellent, 28% had good, 34% had fair and 6% had poor outcomes.[26] Riggins et al, Giles et al, Pritchett JW, and Sanders et al reported the results of distal femoral fractures treated with Dynamic Condylar Screw. Non-union occurred in 0-5.7%, infections in 0-5.3% and malunion in 5.3%-11%.[30], [29], [28], [27] Higher rate of excellent and good results in our series could be probably due to the higher incidence of type A fractures and a lower mean age of patients.
Conclusion
DCS remains a good implant for distal femur fractures particularly types A and B. It is easier to perform, less difficult technically and also cost-effective.
Source of Funding
None.
Conflict of Interest
None.
References
- UE Anyaehie, OC Ejimofor, FC Akpuaka, CU Nwadinigwe. Pattern of femoral fractures and associated injuries in a Nigerian tertiary trauma centre. Niger J Clin Pract 2015. [Google Scholar]
- E Batchelor, C Heal, J K Haladyn, H Drobetz. Treatment of distal femur fractures in a regional Australian hospital. World J Orthop 2014. [Google Scholar]
- H K Doshi, P Wenxian, M V Burgula, D P Murphy. Clinical outcomes of distal femoral fractures in the geriatric population using locking plates with a minimally invasive approach.. Geriatr Orthop Surg Rehabil 2013. [Google Scholar]
- Ashutosh Kumar Singh, Amit Rastogi, Vakil Singh. Biomechanical comparison of dynamic condylar screw and locking compression plate fixation in unstable distal femoral fractures: An in vitro study. Indian J Orthop 2013. [Google Scholar]
- M Ehlinger, G Ducrot, P Adam, F Bonnomet. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res 2013. [Google Scholar]
- M S Butt, S J Krikler, M S Ali. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J Bone Joint Surg Br 1996. [Google Scholar]
- J F Connolly. Closed management of distal femur fractures. Instr Course Lect 1987. [Google Scholar]
- D J Gates, M Alms, M M Cruz. Hinged cast and roller traction for fractured femur. A system of treatment for the third world. J Bone Joint Surg Br 1985. [Google Scholar]
- C S Neer, S A Grantham, M L Shelton. Supracondylar fracture of the adult femur. A study of hundred and ten cases. J Bone Joint Surg Am 1967. [Google Scholar]
- M J Stewart, T D Sisk, S L Wallace. Fractures of the distal third of the femur. J Bone Joint Surg 1966. [Google Scholar]
- J M Siliski, M Mahring, P Hofer. Supracondylar fractures of the femur treated by internal fixation. J Bone Joint Surg 1989. [Google Scholar]
- Brett R. Bolhofner, Barbara Carmen, Philip Clifford. The Results of Open Reduction and Internal Fixation of Distal Femur Fractures Using a Biologic (Indirect) Reduction Technique. J Orthop Trauma 1996. [Google Scholar]
- Keikhosrow Firoozbakhsh, Kambiz Behzadi, Thomas A. DeCoster, Moheb S. Moneim, Fred F. Naraghi. Mechanics of Retrograde Nail Versus Plate Fixation for Supracondylar Femur Fractures. J Orthop Trauma 1995. [Google Scholar]
- George Petsatodis, Apostolos Chatzisymeon, Petros Antonarakos, Panagiotis Givissis, Pericles Papadopoulos, Anastasios Christodoulou. Condylar Buttress Plate versus Fixed Angle Condylar Blade Plate versus Dynamic Condylar Screw for Supracondylar Intra-Articular Distal Femoral Fractures. J Orthop Surg 2010. [Google Scholar]
- Stephen M. David, Matthew E. Harrow, Richard D. Peindl, Steven L. Frick, James F. Kellam. Comparative Biomechanical Analysis of Supracondylar Femur Fracture Fixation: Locked Intramedullary Nail Versus 95-Degree Angled Plate. J Orthop Trauma 1997. [Google Scholar]
- DJ Shewring, BF Meggitt. Fractures of the distal femur treated with the AO dynamic condylar screw. J Bone Joint Surg 1992. [Google Scholar]
- P.J. Radford, C.J. Howell. The AO dynamic condylar screw for fractures of the femur. Injury 1992. [Google Scholar]
- C. Krettek, P. Schandelmaier, T. Nliclau, H. Tscherne. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury 1997. [Google Scholar]
- R P Cusick, G L Lucas, D A Mcqueen, C D Graber. Construct stiffness of different fixation methods for supracondylar femoral fractures. Am J Orthop 2000. [Google Scholar]
- O Martinet, J Cordey, Y Harder, A Maier, M Buhler, G E Barraud. The epidemiology of fractures of the distal femur. Injury 2000. [Google Scholar]
- Brett D. Crist, Gregory J. Della Rocca, Yvonne M. Murtha. Treatment of Acute Distal Femur Fractures. Orthop 2008. [Google Scholar]
- Anil Chander, Ganesan Ram Ganesan, Vignesh Jayabalan. Is Distal Femur Locking Plate a Superior Implant in Distal Femur Fracture?. Open J Orthop 2015. [Google Scholar]
- G. Ramachandra Reddy, P. N. Prasad. Comparison of study of a dynamic condylar screw surgery and distal femoral locking compression plate technique in distal femoral fractures. Int J Res Orthop 2017. [Google Scholar]
- D.G Dunlop, I.J Brenkel. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury 1999. [Google Scholar]
- Robert F. Ostrum, Christoph Geel. Indirect Reduction and Internal Fixation of Supracondylar Femur Fractures Without Bone Graft. J Orthop Trauma 1995. [Google Scholar]
- Kiran P. Paknikar, Shekhar Malve, G. S. Kulkarni, M. G. Kulkarni, S. G. Kulkarni, Anant A. Takalkar. Supracondylar fracture of femur: our experience of treatment with locking compression plate from rural Maharashtra. Int J Res Orthop 2019. [Google Scholar]
- R S Riggins, J G Garrick, P R Lipscomb. Supracondylar fracture of the femur: A survey of treatment. Clin Orthop Relat Res 1972. [Google Scholar]
- J B Giles, J C DeLee, J D Heckman, J E Keever. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw.. J Bone Joint Surg Am 1982. [Google Scholar]
- Pritchett, Jw. Supracondylar fracture of the femur. Clinic Orthop Related Res 1984. [Google Scholar]
- Roy Sanders, Pietro Regazzoni, Thomas P. Ruedi. Treatment of Supracondylar-Intracondylar Fractures of the Femur Using the Dynamic Condylar Screw. Orthop Related Res 1989. [Google Scholar]
