- Visibility 418 Views
- Downloads 152 Downloads
- Permissions
- DOI 10.18231/j.ijos.2024.057
-
CrossMark
- Citation
A prospective study to evaluate the outcome of periarthritis shoulder treated with platelet rich plasma
Abstract
Introduction: Periarthritis shoulder also called as Adhesive capsulitis or Frozen shoulder. The body creates excessive adhesion across the glenohumeral joint as a result of the idiopathic, chronic, and indolent degenerative process known as periarthritis shoulder, which causes discomfort, stiffness, and a reduction in range of motion. In the general population, the prevalence of adhesive capsulitis is 3-55%, and it is 20% in those with diabetes. Many types of treatment have been employed in the treatment of shoulder disorder such as simple analgesia, NSAIDS, intraarticular steroid, platelet rich plasma injection and surgery. PRP is more efficient and long-lasting than cortisone injection for the treatment of adhesive capsulitis, according to several research.
Aims and Objectives: To evaluate the outcome of Periarthritis shoulder treated with Platelet Rich Plasma by comparing the intensity of pain, degree of increase in angle of movements of shoulder.
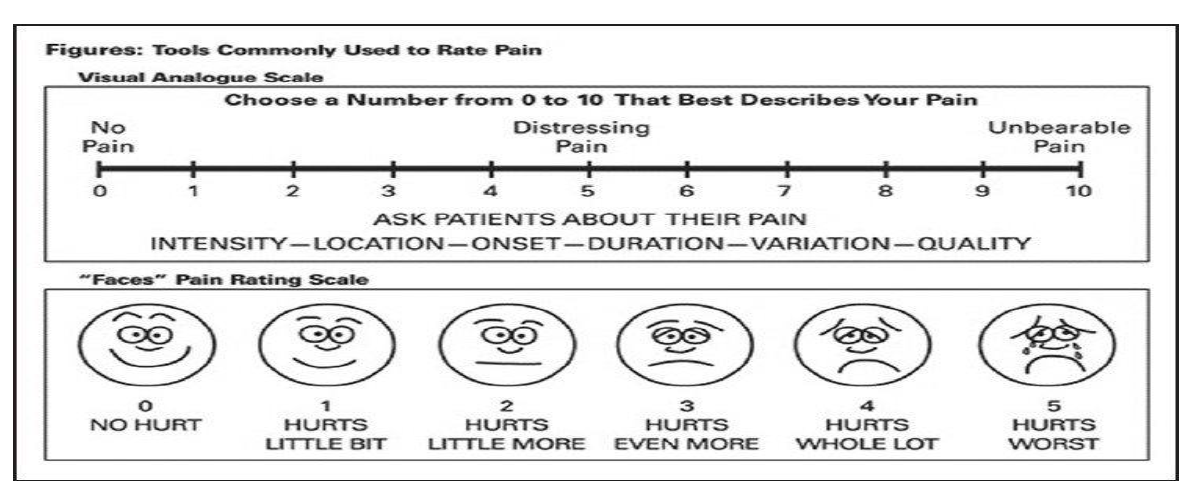
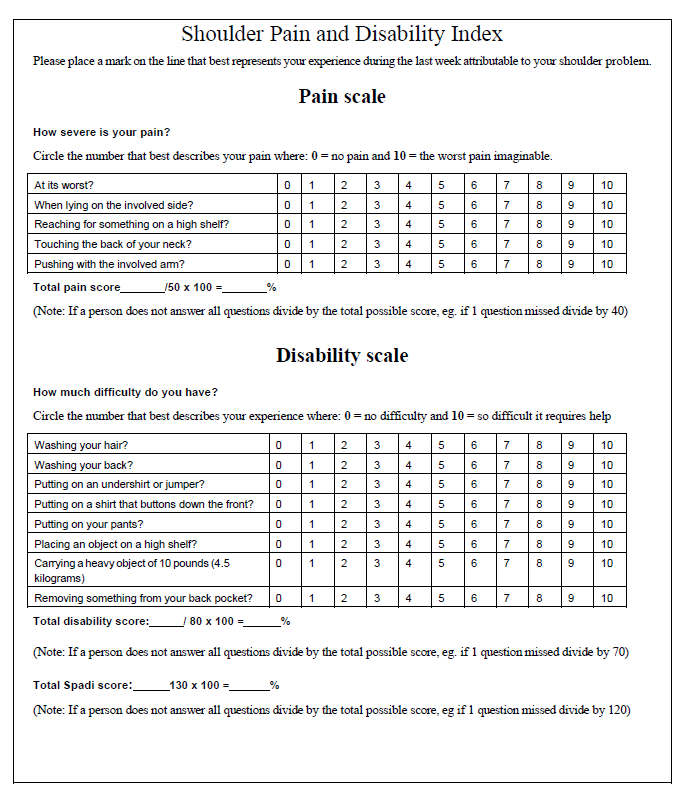
Materials and Methods: It is a randomized control trial with total of 30 patients between age group of 30–70 years old of both sex being diagnosed for the first time and not treated by any other modality are taken up for the study. Patients having chronic pain due to other causes like nerve damage or other neurological disorders, history of fracture around the shoulder joint, patients having local skin infection at the shoulder joint and patient not giving informed consent form to be a part of study were excluded from the study. Under sterile aseptic condition Autologous Platelet Rich Plasma of 4 ml was injected into the shoulder joint. It was a randomized single blinded controlled trial with 1 month, 3 months & 6 months follow up in which outcome was measures using visual analogue scale, ROM, SPADI.
Results: Using the paired t test, descriptive and inferential statistical analysis were performed inthe current study. The mean VAS score at 6 months was reduced from 6.66+2.499 to 3.4±1.473; Mean SPADI Score at 6 month increased from 50.53±14.811 to 76.76±10.926; At 6 month Flexion increased from 66 to 116.33, extension increased from 18.6 to 31.33 and abduction increased from 87.33 to 126.833 with p value of 0.0001 which is statistically significant.
Conclusion: This study concluded that platelet rich plasma injection causes decrease in intensity of pain and increase in angle of movements of shoulder in patients of periarthritis shoulder.
Introduction
Periarthritis shoulder also called as Adhesive capsulitis or Frozen shoulder.[1], [2], [3] The body creates excessive adhesion across the glenohumeral joint as a result of the idiopathic, chronic, and indolent degenerative process known as periarthritis shoulder, which causes discomfort, stiffness, and a reduction in range of motion.[4], [5], [6], [3] It often appears between the ages of 40 and 70. In the general population, the prevalence of adhesive capsulitis is 3-55%, and it is 20% in those with diabetes.[7], [8], [9] Many types of treatment have been employed in the treatment of shoulder disorder such as simple analgesia, NSAIDS, intraarticular steroid, platelet rich plasma injection and surgery.[10], [11], [12], [13], [14], [15]
Although this condition is associated with a number of risk factors, including female sex, trauma, age more than 40, thyroid disease,diabetes, stroke, myocardial infarction, extended mobility andt the existence of an autoimmune disease, the pathophysiology of this disorder is yet unknown.[1], [16], [17], [18], [19]
It's usual to think of adhesive capsulitis as having three phases. The first stage, known as "freezing," is characterised by escalating discomfort and stiffness that may last up to nine months.[20], [21], [22], [23], [24], [25] The second stage, referred to as "frozen," entails a constant condition for a duration of four to twenty month.[26] The third stage, known as "thawing," is a time of spontaneous healing that may last anywhere between five and twenty-six months.[27], [5], [28], [29]
Among the suggested therapies are, intra-articular corticosteroid, benign neglect and hyaluronic acid injections, physical therapy , deep heat modalities, oral corticosteroids, manipulation under anaesthesia, surgical release and hydrodilation.[30], [31], [32], [33], [34] However, the best treatment option is a mater of debate. Due to its physiological effects,USG therapy is used as a treatment, which include, an increase in capillary permeability,increase in blood flow and tissue metabolism, an increase in pain threshold , an improvement in tissue extensibility, and a change in neuromuscular activity that cause relaxation of muscle.[35], [36], [37], [38], [39]
One of the methods often used to treat periarthritis of the shoulder is intra-articular corticosteroid injection.[40], [41], [42], [43], [44], [45] In order to enhance and speed up tendon recovery, PRP has become a novel technique. [46], [47], [48], [49] It is thought to promote the soft tissue revascularisation and growth factors concentration increase. [50], [51], [33], [52] It is described as an autologous blood sample with platelet concentrations exceeding reference levels. [18], [53], [54], [55], [56]
Numerous cytokines and growth like FGF,VEGF PDGF, TGF-beta, EGF, IGF-2, PDGF, and IGF-1, may be found in platelet rich plasma. [57], [58], [59] One of the newer methods of treating this very painful and in capacitating disorder uses keratinocyte growth factors and connective tissue growth factors. [60], [61], [62], [63] Several studies have shown its potential when compared to steroid injection and other forms of conservative therapy. [5], [64], [19], [65]
PRP is more efficient and long-lasting than cortisone injection for the treatment of adhesive capsulitis, according to several research. [66], [67], [34]
The main ideology behind this project is introduction of platelet rich plasma as a biological agent promoting healing when used in the treatment of periarthritis shoulder.
Aims and Objectives
To evaluate thes outcome of periarthritis shoulder treated with platelet rich plasma in the form of:
Intensity of pain reduced after the procedure
Increase in shoulder joint degree of movements
Ability of carrying daily activities without restrictions which the patients were not able to do before.
Materials and Methods
The research was done orthopaedic department of Narayana Medical College & Hospital, Nellore from November 2020 to June 2022 after getting ethical committee clearance.
Inclusion criteria
A total number of 30 patients in the age group of 35-60 years of either sex who are diagnosed with periarthritis shoulder for more than 4 weeks and not relieved by conservative treatment, patients with restricted active and passive movement at glenohumeral joint and patients giving informed consent for study were included in the study.
Exclusion criteria
Patients having chronic pain due to other causes like nerve damage or other neurological disorders, history of fracture around the shoulder joint, patients having local skin infection at the shoulder joint and patient not giving informed consent to be a part of study were excluded from the study and shoulderd pre procedure after 1 month, 3 months and at 6 months.
All the recorded data were interpreted statistically by paired t test and “p” value was calculated to conclude the thesis objectives statistically significant. The data was analyzed using paired t test. Then difference of pain relief between was statistically significant at both 3 months as well as 6 months follow up.
The ROM for Extension, abduction and flexion increased by an average of 12.7 °, 39.5 ° and 40 ° at 6 months follow up showing greater and better increase in ROM of shoulder with PRP.
In our study paired t test was employed to know the efficacy of PRP. Our study inferred that the pain relief was better with PRP at 6 months as compared to 1 month and pre procedure. So over a short term period the pain relief is better with PRP. The difference between pre procedure and 6 months after introducing platelet rich plasma was statistically significant as indicated by the “p” value.
Results
This study included 30 patients, participants were clinically evaluated, a baseline VAS scores, SPADI and ROM were recorded. Out of the 30 participants, 20 (66.66%) were males and 10 (33.33%) were females ([Table 1]).
|
Gender |
Number of cases |
|
Female |
10 |
|
Male |
20 |
|
Total |
30 |
Most of the patients i.e., 21 (70%) in our study were aged between 50-70 years with an average age 59.33 years ([Table 2]).
|
Age (i n years) |
Number of cases |
|
30-40 |
1 |
|
41-50 |
4 |
|
51-60 |
10 |
|
61-70 |
11 |
|
71-80 |
4 |
|
Total |
30 |
|
Mean ± SD |
59.33 ±14.79 |
The mean age was 59.33 years with standard deviation 14.79. The mean duration of the condition in all 30 patients suffering from Adhesive capsulitis was 15.167+10.268 months ([Table 3]).
|
Duration of symptoms (months) |
Number of patients (percentage) |
|
1-5 |
2 (6.66) |
|
6-10 |
4 (13.32%) |
|
11-15 |
10 (33.33%) |
|
16-20 |
6 (19.98%) |
|
21-25 |
6 (19.98%) |
|
26-30 |
1 (3.33%) |
|
31-35 |
1 (3.33%) |
|
Total |
30 (100%) |
|
Mean ± SD |
15.167 ± 10.268 |
Out of 30 participants 1 patient (3.33%) had transient hypotension, 1 (3.33) patient had nausea and 1 patient (3.33%) developed skin rashes along the upper limb after PRP injection ([Table 4]).
|
Complication |
No. of cases |
|
Transient hypotension |
1 (3.33%) |
|
Nausea |
1 (3.33%) |
|
Skin rashes |
1 (3.33%) |
|
Total |
3 (10%) |
The mean VAS score at the presentation was 6.66+2.499. At 1 month these scores reduced to 5.866±1.408 has compared to baseline with p value of 0.131. At 3 months these scores reduced to 5.133±1.384 has compared to baseline with pvalue of 0.004. which is statistically significant. At 6 months these scores significantly reduced to 3.4±1.473 with p value of 0.0001 which is statistically significant ([Table 5]).
|
Time Frame |
Mean |
Standard deviation |
P value |
|
Pre procedure |
6.66 |
2.499 |
|
|
1 months |
5.866 |
1.408 |
0.131 |
|
3 months |
5.133 |
1.384 |
0.004 |
|
6 months |
3.4 |
1.473 |
0.001 |
|
Total |
15.193 |
6.765 |
|
There was a statistically significant reduction inthe VASscore at 1month, 3months and 6months by paired t test.
At 1 month SPADI score was 50.53±14.811 as compared to base line 43.0+14.857 with a p valuer of 0.0616 which is statistically not significant. At 3 months SPADI score was 59.43±14.441 as compared to base line with a value of 0.0001 which is statistically significant. At 6 months SPADI score was 74.76±10.926 as compared to base line with a p value of 0.0001 which is statistically significant ([Table 6]).
|
Time frame |
Mean |
Standard deviation |
P value |
|
Pre procedure |
43.3 |
14.857 |
|
|
1 months |
50.53 |
14.811 |
0.0616 |
|
3 months |
59.43 |
14.441 |
0.0001 |
|
6 months |
74.76 |
10.926 |
0.0001 |
|
Total |
177.49 |
55.025 |
|
After 6 months mean flexion was 116.33 ± 24.964 as compared to pre-procedure of 76 ±19.673 with a p valuer of 0.001 which is statistically significant. After 6 months mean extension was 31.33 ± 8.158 as compared to pre-procedure 18.6 ± 7.846 with a p value of 0.0001 which is statistically significant. After 6 months mean abduction was 126.833 ± 18.325 as compared to base line with a p value of 0.0001 which is statistically significant ([Table 7]).
|
Range of movements |
Time frame |
Mean |
Standard deviation |
P value |
|
Flexion |
Pre procedure |
76 |
19.673 |
|
|
1 Month |
86.16 |
21.043 |
0.062 |
|
|
3 Months |
100.6 |
22.757 |
0.0003 |
|
|
6 Months |
116.33 |
24.964 |
0.0001 |
|
|
Extension |
Pre procedure |
18.6 |
7.846 |
|
|
1 Month |
21.66 |
8.097 |
0.014 |
|
|
3 Months |
25.83 |
9.136 |
0.0017 |
|
|
6 Months |
31.33 |
8.158 |
0.0001 |
|
|
Abduction |
Pre procedure |
87.33 |
21.476 |
|
|
1 Month |
97.66 |
17.547 |
0.0582 |
|
|
3 Months |
108.166 |
16.657 |
0.00001 |
|
|
6 Months |
126.833 |
18.325 |
0.00001 |
Statistical software
For data analysis, the statistical tools SPSS22.0 and Renvironmentver.3.2.2 were utilised, and Microsoft Word and Excel were used to create tables.
Discussion
Most of the patients ages were 40 to 70 years. The average age was 59.33±14.79 years. Kothari et.al., in their study observed that the mean age of all patients was 51.9+10.1 years.[64]
A minor male predominance was seen in this investigation. However, this distinction lacked statistical significance (P=0.825). Crubbs et.al., study showed adhesive capsulitis is more common in middle aged women than males.[52]
The mean duration of symptoms were 15.167+10.268 months. The mean duration of symptoms in all patients was 15.167±10.268 months, which was comparable to a study done by Calis et al., at Turkey in 2019 where mean symptom duration was 5.11±1.90.[48]
At presentation all the demographic and clinical variables in terms of SPADI, ROM in Extension, abduction, flexion was comparable between different follow up periods. At presentation the mean VAS scores was 6.66+4.99. The mean VAS score at the presentation was 66.66+2.499. At 1 month these scores reduced to 5.866±1.408 has compared to baseline with p value of 0.131. At 3 months these scores reduced to 5.133±1.384 has compared to baseline with p value of 0.004 which is statistically significant. At 6 months these scores significantly reduced to 3.4±1.473 with p value of 0.0001 which is statistically significant.
At 3 months follow up the mean VAS score decreased in the groups. Indicating improvement in patients symptoms subjectively. Further at 6 months the mean VAS score decreased very significantly.
The improvement in pain relief and decrease in VAS score in our study was comparable to a study done by Madhan jayaraman et al., at Davanagere in 2018,[11] where it was determined that platelet rich plasma therapy is superior for adhesive capsulitis with 0.001 for VAS score and 0.01 for DASH score, which is statistically significant compared to hydro dissection, and the patients who received it showed improve drange of motion by the end of the first month of follow up.
32 patients who had intra-articular steroid injections for frozen shoulder as part of a research by Rawat et al.[34] exhibited statistically significant pain alleviation after 12 weeks of follow-up. Shah carried out a research on 40 patients, and the results showed a substantial improvement in VAS and CSS ratings with a p-value of 0.05 after 3 doses of intra-articular steroid given at regular intervals. However, in contrast to prior trials, in our research a single dose of steroid injection was administered, and after 12 weeks, the steroid group saw statistically significant pain alleviation.
At 1 month SPADI score was 50.53±14.811 as compared to base line 43.0+14.857 with a p value of 0.0616 which is statistically not significant. At 3 months SPADI score was 59.43±14.441 as compared to base line with a p value of 0.0001 which is statistically significant. At 6 months SPADI score was 74.76±10.926 as compared to base line with a p value of 0.0001 which is statistically significant.
The improvement in SPADI scores in our study was comparable to the improvement in SPADI scores in the study done by Calis et al.,[48] at Turkey which concluded when compared to baseline, there were substantial improvements in the SPADI pain, SPADI disability, and SPADI total scores in functional recovery (p<0.05).
At presentation mean extension was 18.6±7.486. At 1 month the extension improved to 21.66±8.097 with P value of 0.014 which is statistically significant. At 3 months the extension improved to 25.83±9.136 with P value of 0.0017 which is statistically significant. At 6 months the extension improved to 31.33±8.158 with P value of 0.0001 which is statistically significant.
At presentation mean abduction was 87.33±21.476. At 1 month the mean abduction improved to 97.66.±17.547 with P value of 0.0582 which is statistically significant. At 3 months the mean abduction improved to 10.1666±16.657 with P value of 0.00001 which is statistically significant. At 6 months the mean abduction improved to 126.833±18.325 with a P value of 0.0001 which is statistically significant.
At presentation mean flexion was 76±19.673. At 1 month the mean flexion improved to 86.16±21.043 with P value of 0.062 which is statistically significant. At 3 months the mean flexion improved to 100.6±22.757 with P value of 0.0003 which is statistically significant. At 6 months the mean flexion improved to 116.33±24.964 with a P value of 0.0001 which is statistically significant.
The ROM for extension abduction and flexion increased by an average of 12.7 °, 39.5 ° and 40 °. at 6 months follow up showing greater and better increase in ROM at shoulder with PRP group. The improvement in ROM in our study was compared with a study done by Kothari et al.,[64] at Delhi in 2017 which concluded, At 12 weeks, passive aswellas active range of motion of the should era, discomfort (VAS) and function all showed statistically significant improvements after PRP treatment compared to corticosteroid and ultrasonic therapy. Also according to a study done by Aslani et al.[22] reported 60% improvement in pain, 70% improvement in functional outcome, where flexion improved from 70º to 150º, abduction improved from 75º to 135º, and external rotation improved from 25º to 50º. He also reported a 70% satisfaction score after treatment with PRP injection inpatients suffering with adhesive capsulitis. Which is comparable to our present study in terms of functional outcome in ROM, SPADI, scores and VAS scores.
Significantly more patients (92.50%) reported total pain relief after six months of follow-up. The current study outcomes were comparable to a similar study done by Kothari et al.,[64] at Delhi in 2017, which concludes passive aswellas active range of motion of the shoulder, quick DASH, VAS and all showed statistically significant improvements after PRP treatment at 12 weeks compared to corticosteroid and ultrasonic therapy.
Conclusion
Hence we concluded that intra articular introduction of platelet rich plasma in periarthritis shoulder showed reduction in the intensity of pain, increase in angle of movements of shoulder joint and improvement in ability of carrying daily activities without restrictions which the patients were not able to do before.
Ethical Approval
This study was approved by Institute Ethical approval Committee with ref. No. NMC/ Adm/ Ethics/ approval/ 094/ 2021.
Conflict of Interest
None.
Source of Funding
None.
References
- Neviaser J. Adhesive capsulitis of the shoulder: A study of the pathological findings in periarthritis of the shoulder. J Bone Joint Surg Am. 1945;27(2):211-22. [Google Scholar]
- Binder A, Bulgen D, Hazleman B, Roberts S. Frozen shoulder: A long-term prospective study. Ann Rheum Dis. 1984;43(3):361-4. [Google Scholar]
- Charnley J. Periarthritis of the shoulder. Postgrad Med J. 1959;35(405):384-8. [Google Scholar]
- Lloyd-Roberts G, French P. Periarthritis of the shoulder: a study of the disease and its treatment. Br Med J. 1959;20(1):1569-71. [Google Scholar]
- Grey R. The natural history of "idiopathic" frozen shoulder. J Bone Joint Surg Am. 1978;60(4). [Google Scholar]
- Terry G, Chopp T. Functional anatomy of the shoulder. J Athl Train. 2000;35(3):248-55. [Google Scholar]
- Carmichael S, Hart D. Anatomy of the shoulder joint. J Orthop Sports Physical Therapy. 1985;6(4):225-8. [Google Scholar]
- . Anatomy, Function, and Dysfunction of the Shoulder Complex. The Shoulder Section III: the upper extremities. . [Google Scholar]
- Hsu W, Mishra A, Rodeo S, Fu F, Terry M, Randelli P. Platelet-rich plasma in orthopaedic applications: evidence-based recommendations for treatment. J Am Acad Orthop Surg. 2013;21(12):739-48. [Google Scholar]
- Uppal H, Evans J, Smith C. Frozen shoulder: A systematic review of therapeutic options. World J Orthop. 2015;6(2):263-8. [Google Scholar]
- Carr B, Canapp S, Canapp D, Gamble L, Dycus D. Adhesive Capsulitis in Eight Dogs: Diagnosis and Management. Front Vet Sci. 2016;3. [Google Scholar]
- Shekhar V, Reddy G. Role of Intra Articular Steroid Injection In Early Adhesive Capsulitis of Shoulder. IOSR J Dent Med Sci (IOSR- JDMS. 2017;16(3):38-40. [Google Scholar]
- Widiastuti-Samekto M, Sianturi G. Frozen shoulder syndrome: comparison of oral route corticosteroid and intra-articular corticosteroid injection. Med J Malaysia. 2004;59(3):312-6. [Google Scholar]
- Çalış H, Karabaş �, Güler E. Effects of Platelet-rich Plasma Injection on Adhesive Capsulitis: An Interventional Case Series. Erciyes Med J. 2019;41(1):102-4. [Google Scholar]
- Jeyaraman M, Ramesh R, Prajwal G, Dhamsania H. The comparative and prospective study on efficacy and functional outcome of autologous platelet rich plasma injection vs hydrodissection in adhesive capsulitis of shoulder. Int J Res Orthop. 2018;4(6):1-6. [Google Scholar]
- Binder A, Bulgen D, Hazleman B, Roberts S. Frozen shoulder: a long-term prospective study. Ann Rheum Dis. 1984;43(3):361-4. [Google Scholar]
- Milgrom C, Novack V, Weil Y, Jaber S, Radeva-Petrova D, Finestone A. Risk factors for idiopathic frozen shoulder. Isr Med Assoc J. 2008;10(5):361-4. [Google Scholar]
- Lim T, Koh K, Shon M, Lee S, Park Y, Yoo J. Intra-articular injection of hyaluronate versus corticosteroid in adhesive capsulitis. Orthopedics. 2014;37(10):860-5. [Google Scholar]
- Dhurat R, Sukesh M. Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author's Perspective. J Cutan Aesthet Surg. 2014;7(4):189-97. [Google Scholar]
- Shaffer B, Tibone J, Kerlan R. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am. 1992;74(5):738-46. [Google Scholar]
- Parker R, Froimson A, Winsberg D, Arsham N. Frozen Shoulder: Part I: Chronology, Pathogenesis, Clinical Picture and Treatment. Orthopedics. 1989;12(6):869-73. [Google Scholar]
- Rizk T, Pinals R. Frozen shoulder. Semin Arthritis Rheumatism. 1982;11(4):440-52. [Google Scholar]
- Friedman N, Laban M. Periarthrosis of the shoulder associated with diabetes mellitus. Am J Phys Med Rehabil. 1989;68(1):12-4. [Google Scholar]
- Bunker T, Anthony P. The pathology of frozen shoulder. A Dupuytren-like disease. J Bone Joint Surg Br. 1995;77(5):677-83. [Google Scholar]
- Ozaki J, Nakagawa Y, Sakurai G, Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71(10):1511-5. [Google Scholar]
- Sun Y, Zhang P, Liu S, Li H, Jiang J, Chen S. Intra-articular Steroid Injection for Frozen Shoulder: A Systematic Review and Meta-analysis of Randomized Controlled Trials With Trial Sequential Analysis. Am J Sports Med. 2017;45(9):2171-9. [Google Scholar]
- Rodeo S, Hannafin J, Tom J, Warren R, Wickiewicz T. Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J Orthop Res. 1997;15(3):427-36. [Google Scholar]
- Rizk T, Pinals R. Histocompatibility type and racial incidence in frozen shoulder. Arch Phys Med Rehabil. 1984;65(1):33-4. [Google Scholar]
- Vinores S, Campochiaro P. Prevention or moderation of some ultrastructural changes in the RPE and retina of galactosemic rats by aldose reductase inhibition. Exp Eye Res. 1989;49(3):495-510. [Google Scholar]
- Levine W, Kashyap C, Bak S, Ahmad C, Blaine T, Bigliani L. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007;16(5):569-73. [Google Scholar]
- O'kane J, Jackins S, Sidles J, Smith K, Matsen F. Simple home program for frozen shoulder to improve patients' assessment of shoulder function and health status. J Am Board Fam Pract. 1999;12(4):270-7. [Google Scholar]
- Hertling D, Kessler R. . Management of Common Musculoskeletal Disorders: Physical Therapy Principles and Methods. 2006. [Google Scholar]
- Malavolta E, Gracitelli M, Sunada E, Benegas E, Prada F, Neto R. Platelet-rich plasma in arthroscopic repairs of complete tears of the rotator cuff. Rev Bras Ortop. 2015;47(6):741-7. [Google Scholar]
- Rawat M, Juyal A, Agarwal A. Evaluation of the role of intra-articular steroid injection in frozen shoulder. Int J Orthop Sci. 2018;4(1):792-4. [Google Scholar]
- Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005;331(7530):1453-6. [Google Scholar]
- Sonal C, Kothari S, Nonica L. . Comparison of ultrasonic therapy, sodium hyaluronate injection and steroid injection in the treatment of peri-arthritis shoulder. 2012;23:105-115. [Google Scholar]
- Neviaser A, Hannafin J. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010;38(11):2346-56. [Google Scholar]
- RC, MF. Murnaghan lP: Frozen shoulder. The Shoulder. 1990. [Google Scholar]
- Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010;5(4):266-73. [Google Scholar]
- Griesser M, Harris J, Campbell J, Jones G. Adhesive capsulitis of the shoulder: a systematic review of the effectiveness of intra-articular corticosteroid injections. J Bone Joint Surg Am. 2011;93(18):1727-33. [Google Scholar]
- Blanchard V, Barr S, Cerisola F. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy. 2010;96(2):95-107. [Google Scholar]
- Koh K. Corticosteroid injection for adhesive capsulitis in primary care: a systematic review of randomised clinical trials. Singapore Med J. 2016;57(12):646-57. [Google Scholar]
- Frank R. Sorbinil and limited joint mobility in diabetics. JAMA. 1985;254(11):1452-4. [Google Scholar]
- Hand G, Athanasou N, Matthews T, Carr A. The pathology of frozen shoulder. J Bone Joint Surg. 2007;89(B):928-32. [Google Scholar]
- Ryans I, Montgomery A, Galway R, Kernohan W, Mckane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatol. 2005;44(4):529-35. [Google Scholar]
- Buchbinder R, Hoving J, Green S, Hall S, Forbes A, Nash P. Short course prednisolone for adhesive capsulitis (frozen shoulder or stiff painful shoulder): a randomised, double blind, placebo controlled trial. Ann Rheum Dis. 2004;63(11):1460-9. [Google Scholar]
- Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4(4):193-6. [Google Scholar]
- D’orsi G, Via A, Frizziero A, Oliva F. Treatment of adhesive capsulitis: a review. Muscles Ligaments Tendons J. 2012;2(2):70-8. [Google Scholar]
- Mukherjee R, Pandey R, Nag H, Mittal R. Frozen shoulder-A prospective randomized clinical trial. World J Orthop. 2017;8(5):394-9. [Google Scholar]
- Kozin F. Two unique shoulder disorders. Adhesive capsulitis and reflex sympathetic dystrophy syndrome. Postgrad Med. 1983;73(5):207-10. [Google Scholar]
- Fukaya M, Ito A. A New Economic Method for Preparing Platelet-rich Plasma. Plast Reconstr Surg Glob Open. 2014;2(6). [Google Scholar]
- Crubbs N. Frozen shoulder syndrome: a review of literature. J Orthop Sports Phys Ther. 1993;18(3):479-87. [Google Scholar]
- Marx R, Malizia R, Kenter K, Wickiewicz T, Hannafin J. Intra-articular corticosteroid injection for the treatment of idiopathic adhesive capsulitis of the shoulder. HSS J. 2007;3(2):202-7. [Google Scholar]
- Jong BD, Dahmen R, Hogeweg J, Marti R. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehabil. 1998;12(3):211-5. [Google Scholar]
- Sakeni R, Al-Nimer M. Comparison between intraarticular triamcinolone acetonide and methylprednisolone acetate injections in treatment of frozen shoulder. Saudi Med J. 2007;28(5):707-12. [Google Scholar]
- Choi H, Kim S, Kim C, Choi H, Shin D, Uhm K. The Cheapest and Easiest Way to Make Platelet-rich Plasma Preparation. Arch Aesthet Plast Surg. 2015;21(1):12-7. [Google Scholar]
- Eppley B, Woodell J, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114(6):1502-8. [Google Scholar]
- Tanishima T, Yoshimasu N. Development and prevention of frozen shoulder after acute aneurysm surgery. Surg Neurol. 1997;48(1):19-22. [Google Scholar]
- Andrén L, Lundberg B. Treatment of rigid shoulders by joint distension during arthrography. Acta Orthop Scand. 1965;36(1):45-53. [Google Scholar]
- Scibek J, Carcia C. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J Orthop. 2012;3(6):87-94. [Google Scholar]
- Codman E. . The shoulder : rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. 1934. [Google Scholar]
- Duplay E. De la périarthrite scapulo-huméral et des raideurs de l'epaule qui en son la conséquence. Arch Gén Méd. 1872;20:513-513. [Google Scholar]
- Aslani H, Nourbakhsh S, Zafarani Z, Ahmadi-Bani M, Ananloo M, Beigy M. Platelet-rich plasma for frozen shoulder: A case report. Arch Bone Jt Surg. 2016;4(1):90-3. [Google Scholar]
- Kothari S, Srikumar V, Singh N. Comparative efficacy of platelet rich plasma injection, corticosteroid injection and ultrasonic therapy in the treatment of periarthritis shoulder. J Clin Diagn Res. 2017;11(5):15-8. [Google Scholar]
- Agrawal A, Nayak B, Sakale H. Management of Adhesive Capsulitis of Shoulder Joint by Single Platelet Rich Plasma Injection. J Orthop Traumatol Rehabil. 2019;11(1):62-5. [Google Scholar]
- Kim Y, Lee G. Immediate Effects of Angular Joint Mobilization (a New Concept of Joint Mobilization) on Pain, Range of Motion, and Disability in a Patient with Shoulder Adhesive Capsulitis: A Case Report. Am J Case Rep. 2017;18:148-56. [Google Scholar]
- Perez A, Lana J, Rodrigues A, Luzo A, Belangero W, Santana M. Relevant aspects of centrifugation step in the preparation of platelet-rich plasma. ISRN Hematol. 2014;2014. [Google Scholar]
How to Cite This Article
Vancouver
Yadav VR, Ravindran B, Vardhan NV, Jyothsna RV. A prospective study to evaluate the outcome of periarthritis shoulder treated with platelet rich plasma [Internet]. Indian J Orthop Surg. 2024 [cited 2025 Oct 06];10(4):351-357. Available from: https://doi.org/10.18231/j.ijos.2024.057
APA
Yadav, V. R., Ravindran, B., Vardhan, N. V., Jyothsna, R. V. (2024). A prospective study to evaluate the outcome of periarthritis shoulder treated with platelet rich plasma. Indian J Orthop Surg, 10(4), 351-357. https://doi.org/10.18231/j.ijos.2024.057
MLA
Yadav, Vinod Ramlal, Ravindran, Biju, Vardhan, N Vishnu, Jyothsna, Rachuru Venkata. "A prospective study to evaluate the outcome of periarthritis shoulder treated with platelet rich plasma." Indian J Orthop Surg, vol. 10, no. 4, 2024, pp. 351-357. https://doi.org/10.18231/j.ijos.2024.057
Chicago
Yadav, V. R., Ravindran, B., Vardhan, N. V., Jyothsna, R. V.. "A prospective study to evaluate the outcome of periarthritis shoulder treated with platelet rich plasma." Indian J Orthop Surg 10, no. 4 (2024): 351-357. https://doi.org/10.18231/j.ijos.2024.057
