Introduction
Subtrochanteric fracture femur has been variously defined, many authors limit the term to fractures between the lesser trochanter and the isthmus of the diaphysis.1
In the last 50 years, the treatment of subtrochanteric femur fractures have evolved with increased understanding of both the fracture biology and biomechanics. Previously, nonsurgical treatment of these fractures were associated not only with significant malrotation and shortening, but also with morbidity and mortality associated with prolonged immobilization.
The difficult nature of treating subtrochanteric fracture stems in part from the fact that this injury pattern is anatomically distinct from other proximal femoral peritrochanteric fractures and also from the femoral shaft fractures. As a result, it must be treated with specially designed implants which can withstand significant muscular forces for longer periods of healing. These stronger muscular forces deform the fracture fragments and make reduction difficult and as comminution is common in subtrochanteric region the implant must withstand significant early loading.
The combination of tensile, compression and torsional stresses in the region has challenged orthopaedicians with problems of delayed union and nonunion, and resulting in loss of fixation, implant failure, and iatrogenic devascularization of the operative exposure.
Only recently has a better understanding of fracture biology, reduction techniques, and biomechanically improved implants has allowed subtrochanteric fractures to be addressed with some success.
In 1996, the proximal femoral nail (PFN) was developed,2,3 used as an intramedullary device for the treatment of such fractures. In addition to all advantages of an intramedullary nail, it has several other favourable characteristics like it can be dynamically locked, allows early mobilization, has high rotational stability and is done with minimal soft tissue damage. With this a study was taken to analyse the union of the subtrochanteric fracture, internally fixed with PFN.
Materials and Methods
Study was conducted in the department of orthopaedics, GSL Medical College. Study protocol was approved by the institutional ethics committee; informed written consent was taken from the study participants.
Individuals with acute subtrochanteric femur fractures >18 years were included in the study. Fractures in patients below the age of 18 years, open fractures and pathological subtrochanteric femur fractures were not considered. All patients were maintained on traction before surgery. All surgeries were done under spinal or epidural anaesthesia. Low molecular weight heparin prophylaxis was given subcutaneously for the high risk patients during the hospitalization. The length of hospital stay, any blood transfusions or hospital acquired complications were recorded.
When the subtrochanteric fractures occurred because of high energy trauma, polytrauma management dominates the initial fracture treatment. The life-threatening conditions must be adequately handled before managing the definitive treatment of the subtrochanteric fracture. In severely injured patients, the concept of damage control in the acute management must be considered and practiced. Non-operative treatment is only indicated in the paediatric age group or in patients who are not fit for surgery under anesthesia. With the advancement of anesthesia technology and intraoperative monitoring, most of the patients can undergo surgery with predictable outcomes. The closed method follows the principle of anatomical realignment in which deformities in length and rotation are corrected to achieve a result that is as normal as possible. This procedure is applied with closed reduction and internal fixation.4 The PFN was developed by AO/ASIF. The Indian versions are available and have been used in our study.2,3
The patient was positioned supine on the fracture table under spinal or epidural or general anesthesia as the condition of the patient permitted. Pre-operatively one dose of antibiotic was also administered. The fracture was reduced by longitudinal traction on fracture table and the limb was placed in neutral or slight adduction to facilitate nail insertion through the greater trochanter (Figure 2). Prior to positioning and draping, the opposite extremity measurements of rotation and length of this extremity were determined. Post operative results were assessed by Harris Hip score.
Statistical analyses were done by using SPSS software version 21.0. Chi-square test was used to assess the association between different categorical variables; P<0.05 was considered statistically significant.
Results
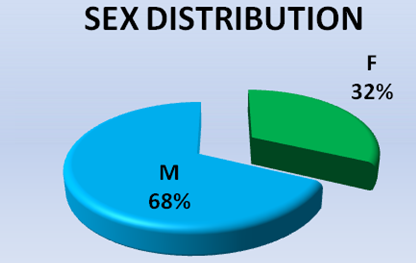
Total 25 patients were included in this study ; patients were distributed across all age groups, one patient above the age of seventy years (Table 1); 17 were male patients and 8 female patients (Figure 2).
The average duration of hospital stay was 17.64 days, ranged 14 to 23 days. At the end of five months, except three patients remaining could mobilize independently. One patient with a contralateral intertrochanteric fracture was using a Zimmer frame to mobilise. Two patients were using crutches to mobilize up to six months postoperatively (Table 2). statistically there was significant difference (P<0.05). Based on Harris Hip score obtained 3 patients outcome was excellent, 18 patients were good and 4 patients had fair outcome (Table 3).
Table 1
| Age | Participants |
| 18 – 30 | 7(28) |
| 31 – 50 | 9(36) |
| 51 – 70 | 8(32) |
| > 70 | 1(4) |
| Total | 25(100) |
Age distribution of the study participants; n (%)
Table 2
| Task | 12 weeks | 20 weeks | 24 weeks |
| Walk Independently | 3(12) | 22(88) | 25(100) |
| Crutch | 12(48) | 2(8) | Nil |
| Zimmer Frame | 10(40) | 1(4) | Nil |
Postoperative independence of ambulation; n (%)
Discussion
In modern trauma care, there is no role of the conservative treatment, as advocated by Delee et al.5 The treatment choices for femoral subtrochanteric fractures can be divided into cepholomeduallary hip nails and lateral plate-screw systems.
The dynamic compression hip screw has been a popular method of internal fixation for subtrochanteric fractures of the femur.6,7 It provides compression along the femoral neck, and if the fracture reduction is stable, load-sharing occurs between the bone and implant.8 But, if stable reduction with postero medial continuity and compression is not achieved, there will be progressive medial displacement of the femoral shaft, which results in loss of bony contact and fixation failure and nonunion. If medialization of more than one-third of the femoral diameter at the fracture site occurs there is sevenfold increase of failure rate.9 The use of intramedullary nail in peritrochanteric fractures has been increasing, and more scholars choose it because it is easy and fast to apply and can give stability even in inherently unstable fractures.10,11
The average length of Hospital stay was 17.6 days. At the end of five months, all except three patients could mobilise independently without any aid. One patient with a contralateral Intertrochanteric fracture femur was using a Zimmer frame to mobilise. Other two patients was using a crutch to mobilise up to six months postoperatively. One patient had a superficial infection at the surgical wound site which subsided with parenteral antibiotics. None of the cases needed a reoperation.
According to harris hip score and our assessment criteria 3 patients had excellent outcome, 18 patients had good outcome and 4 patients had fair outcome. We feel that the PFN is a better implant in treating subtrochanteric fracture of femur. However, a comparative study with the other implants would be appropriate to make definitive conclusions.
Open reduction in irreducible fractures is described in many papers. 80% of our cases reduction was possible with closed method and only 20% cases we needed to open to achieve length, rotation and satisfactory angulation. While study conducted by Kanthimathi et al., has reported that 78% are reduced by closed method and 22% by open method.12 May be this disparity is because of the sample character differing in between the two studies.
Short PFN were used for the type 1a and 1b, 2a fractures following B.F. Ongkiehong A et al., stating that minimum distance between distal screw and fracture site should be 4 to 5 cm.13 Rest of fracture types where comminution is present and the fracture is at lower level long PFN used as implant of choice.
Baumgaertner et al., described that the tip-to-apex distance to be useful intraoperative indicator of deep and central placement of the lag screw in the femoral head, to fix the fracture. This is most important measurement of accurate placement and has been shown in multiple studies to be predictive of success.14 In our study the lag screw of the PFN placed in the lower part of the femoral neck, close to the femoral calcar, with the screw tip reaching the subchondral bone, 10 mm below the articular cartilage in the AP view and In the lateral view placed in the centre of the femoral neck keeping the tip apex distance within acceptable limit of less than 25 mm. The derotation screw 10 mm shorter than lag screw was preferred in most studies.
In one case we could not pass the second screw because of the small neck similar to the experience of Kamboi et al this patient had progressed to radiological union but with the development of screw back out and cut through almost to the superior cortex.15 One case derotation screw had become longer and it has shown a z effect, cut through near to superior cortex but ultimately progressed to union with varus and shortening this patient had to be kept non weight bearing for a prolonged time. In this case we followed the regular recommendation of 10 mm lesser screw than lag screw. Post operative radiograph showed that the derotation screw is higher than the lag screw, when a horizontal line drawn from the tip of lag screw. This indicates that not only one should consider 10 mm shorter screw while selecting a derotation screw but also that it should not be placed higher than the lag screw when we draw a horizontal, which places the derotation screw in weight bearing position instead of lag screw.
The reduced fractures are fixed with stable internal fixation to allow early mobilization. To facilitate fracture healing, the technique of internal fixation must follow the guidelines of minimizing the trauma to the soft tissues and the osseous fragments. Plating of subtrochanteric region through lateral a pproach of the proximal femur, the vastus lateralis muscle must be split or elevated off the intermuscular septum close to large perforating branches of the profunda femoris artery. Division of these vessels causes copious bleeding, making surgical exposure difficult. With proximal femoral nail exposure of lateral aspect of femur is minimal thus avoiding unnecessary blood loss and fracture hematoma remains undisturbed in 80 % of cases which can be reduced in closed manner which helps in hastening the union of bone.
Average time for radiological union in our study is 19 weeks (4.8 months). Radiological union in other studies was 19 weeks, 18 weeks and 12.6 weeks respectively by Ashish et al., Prasad M.Gowda et al., and B Kanthimathi et al.,12,16,17 Our results of achieving union in 19 weeks are at par with the rest of the studies. Patients are encouraged to sit and start quadriceps exercises, on the first post operative day. On second post operative day, patients with no comminution, transverse and short oblique fractures are allowed to start partial weight bearing with walker support and gradually converted to weight bearing as tolerated.
Conclusion
PFN is a good implant for subtrochanteric fracture of the femur. Minimal exposure (closed technique), better stability and early mobilization are the advantages. Fractures united in all cases and postoperative functional outcome was satisfactory. PFN could be a preferred implant of choice in treating subtrochanteric fractures especially in elderly since it allows early and stable mobilization. However, a larger study may be desirable.