- Visibility 106 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijos.2020.012
-
CrossMark
- Citation
Study on outcome of cemented total hip replacement by posterolateral approach to hip
- Author Details:
-
Rahul Modi *
-
Jayant Thipse
Introduction
Displaced subcapital and intracapsular femoral neck fractures unsuitable for reduction and primary fixation are usually treated in elderly with an arthroplasty procedure.[1]
Blomfeldt et al.[2] randomized 120 patients to have either cemented THR or cemented bipolar hemiarthroplasty. Duration of surgery was longer in the THR group and the blood loss was significantly higher, but this was not associated with any increase in the rate of postoperative complications. There were no dislocations in either group. At 4 months and 12 months postoperatively, hip function as measured by Harris hip score was significantly better in the THR group.[3]
A recent meta-analysis concluded that total hip replacement may lead to lower reoperation rates and better functional outcomes compared with hemiarthroplasty and this is supported by the recent update to guidance in Scotland.[4], [5]
Avascular necrosis (AVN) head of femur is an extremely debilitating disease due to multifactorial etiology occuring in relatively younger patients. It results in a collapse of necrotic segment leading to loss of congruence and subsequently degenerative arthritis of the hip joint.[6]
AVN of head of femur forms one of the major indications for total hip replacement. Between 5-12% of the total hip replacements are performed in patients who have AVN of femoral head.[7]
In advanced osteoarthritis of the hip there will be painful gross limitation of movements incapacitating individual from his routine activities. This study of cemented total hip replacement is a boon to these patients by painless mobility of the joint.
In rheumatoid arthritis which is an autoimmune disorder will be causing gross limitation and severely painful joint movements. Cemented Total hip replacement will improve the outcome of life.
Early hip replacements, carried out in the 1950s, were inserted into bone without the use of bone cement. In the early 1960s, Charnley introduced the concept of using acrylic bone cement to fix the prosthesis in place.[8]
Cemented femoral component provides an immediate postoperative advantage (i.e. of intimate contact between the prosthesis cement and the bone, which permits dramatic early relief of pain and more weight – bearing).
The posterolateral approach is a modification of posterior approaches described by Gibson and by Moore. The approach can be extended proximally by osteotomy of the greater trochanter with anterior dislocation of the hip. The approach can be extended distally to allow a posterolateral approach to the entire femoral shaft. We use the posterolateral approach for primary and revision total hip replacement.[9]
This study is intended to bring out various advantages and disadvantages in cemented total hip replacement, its technical difficulties and clinical outcome.
Aims and Objectives
To study the clinical outcome of cemented total hip replacement surgery.
To study the functional outcome of cemented total hip replacement surgery.
To study the complications.
To compare the results of this study with reported studies.
To study the advantages and disadvantages of this technique.
Materials and Methods
In this study 40 patients with 49 hips, aged between 34 and 76 years, with diseased and destroyed hips were treated with cemented total hip replacement at a tertiary care hospital in a rural setup from Jan 2016 to June 2017. The follow up was for a minimum period of 6 months.
Materials
Electronic operation table
Lateral post..
Bone saw.
All implants required for cemented total hip replacement.
Goniometer.
Measuring tape.
Inclusion criteria
Patients with Fracture Neck of Femur of either sex.
MRI evidence of Grade 3 or more Avascular Necrosis of Head of Femur of either sex.
Advanced Rheumatoid arthritis not responding to conservative management of either sex.
Advanced Osteoarthritis not responding to conservative management of either sex.
Exclusion criteria
Active infection of hip joint or any other region.
Rapidly progressive neurological diseases, for e.g.:- Parkinsonism.
Absence or relative insufficiency of the abductor mechanism.
Associated bleeding/coagulation disorders.
Method
Procedure of cemented total hip replacement is carried out in major operation theater as 1st case under all aseptic precautions under spinal/epidural/general anesthesia after pre-anesthetic fitness using posterolateral approach to hip with patient in semi prone position with injured side up. Procedure done under antibiotic cover followed by post op antibiotics.
Surgical approach and technique
The Moore’s approach was followed for all the cases.
The advantage of this approach is that it is a safe and easy approach and has lesser risk of damage to neurovascular structures except the sciatic nerve.
A disadvantage to this approach is the higher rate of dislocation, reported to be as high as 9.5%.[10], [11]
Positioning - Stable position on true lateral decubitus is a must to avoid malpositioning of implants.

Preparation and draping - The first assistant who has scrubbed and applied sterile gloves prepares the lower limb from a level well proximal to the umbilicus and including the groin and anteromedial part of opposite thigh. The foot is held by another assistant who now abducts the limb thereby elevating the buttock which is prepared. The first assistant uses a pad to hold the ankle and thereby prepares the foot and toes.

After this adductor tenotomy, if needed, is done in a sterile condition. Following this, the surgical team proceed with the sterile draping of the limb. Four double sheets along with an adhesive sheet are used to isolate the lower limb from the perineum and rest of the body providing atleast four layers of drapes and isolating the head end of the patient and anaesthetist from the field.

The lower limb is now received into two sets of double towels and bandaged. A stockinette is then applied over the entire lower limb upto the pelvis. The stockinette is then cut over the skin incision site.

An iodine coated adhesive sheet is now applied to the exposed skin and surrounding drapes.
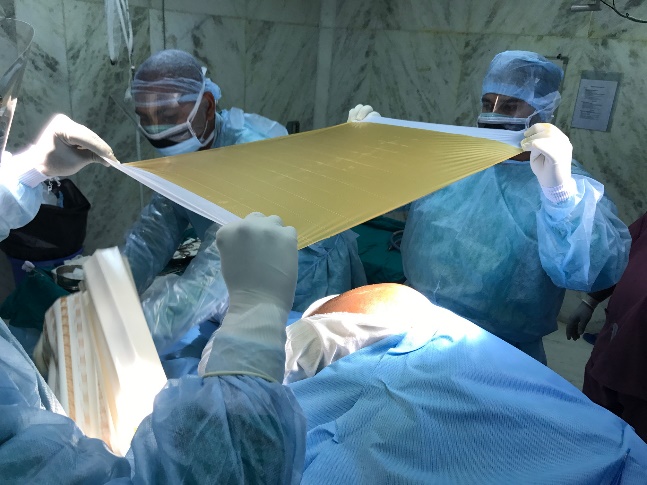
The surgeon and his assistants wore wrap around gowns after scrubbing. Trolley is made ready with all the necessary implants and instruments on the trolley after autoclaving.

Technique
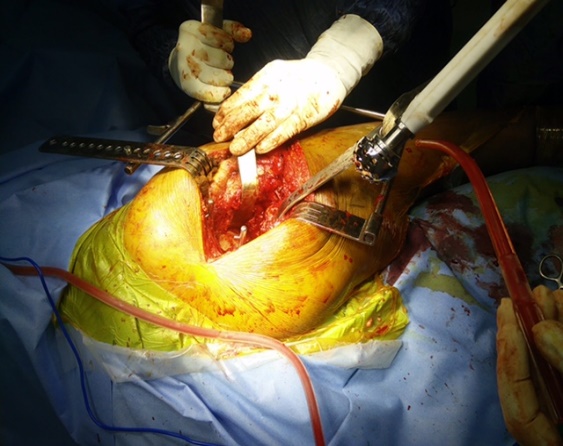
The incision, superficial and deep dissection was done as per the Moore’s approach and self-retaining Charnley’s retractor is applied for good exposure.

The trochanteric bursa is excised and piriformis is cut and the femoral head is exposed after incising the capsule. Short external rotators are tagged and cut flush to the bone. The head is dislocated by flexion, adduction and internal rotation. If internal rotation was restricted a capsular and psoas release was done for facilitation of the rotation and dislocation of the hip.
The neck cut is taken at pre-planned level using saw.

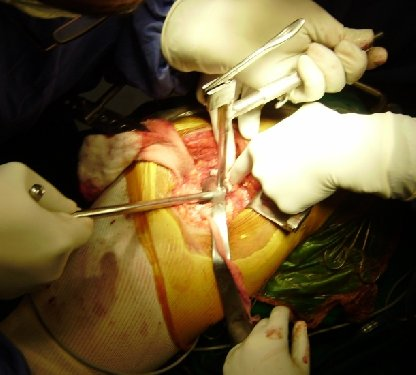
For acetabular exposure, anterior swan neck retractor was placed along anterior lip of acetabulum after making a capsular opening. Hohman's retractor are placed below transverse ligament. Posterior soft tissues are retracted with a right angle retractor or posterior cobra retractor with hip in extension. Excision of capsule and labrum is completed to provide 360 degrees exposure of the bony margins of the rim of acetabulum.
Osteophytes that protrude beyond the bony limits of true acetabulum are removed. Fibrofatty tissue, ligamentum teres and medial/inferior osteophytes are excised to expose medial wall of acetabulum. This depth indicates the limit to which acetabulum can be safely deepened. Direction of reamer is 45 degrees to longitudinal axis of body and 15 degrees of anteversion.
Reaming is completed when all cartilage is removed and reamer has cut bone out to the periphery of acetabulum to expose bleeding subchondral bone.

Appropriate sized trial cup is placed in 45-50 degrees of inclination. Orientation and containment of the cup were noted.
For preparation of the femur, femur was rotated internally so that tibia is perpendicular to floor while covering the acetabulum with a sponge. Proximal femur is delivered from the wound by pushing on the knee and keeping a toothed cobra retractor below the neck. Soft tissue from lateral aspect of neck and piriformis fossa is removed with a nibbler. Bone is removed from lateral portion of neck and medial aspect of greater trochanter to form a groove. This prevents varus placement of the prosthesis. Box punch is used to make the entry and appropriate anteversion of the femoral component. Canal finder is used to enter the medullary canal and by directing it towards the medial femoral condyle. Successive sized rasps are used for the femoral canal preparation.

The trial stem, cup and head is inserted and trial reduction is done. Range of movements, stability of the joint and limb length correction were noted. Schuck test and co-planar tests were done for confirmation of the stability and the length. Not more than 5 mm separation should be present on traction on the limb.

The acetabular cup placement is done. Cement mixing is started when the acetabulum has been reamed appropriately and floor is ready and final implant size has been selected.

Cup is attached to holder in the correct orientation of long posterior wall and final implantation is done with cement. After the cement is mixed, its setting goes through three stages i.e. hairy stage, scrotal stage and doughy stage. The cement is inserted when it reaches the doughy stage where the cement doesn’t stick to the gloves. Use fingers to push cement into anchor holes. The cup clipped to cup holder is pushed into the depth of acetabulum pressing on to the cement with cup holder directed toward the patient's foot. Cup pusher is then positioned in to the depression in the cup holder to keep the cup in the depth of acetabulum while the handle is brought up towards patient's head. Handle is brought into final orientation where the transverse arm is parallel to transverse axis of pelvis and 5 to 10 degrees anteversion.
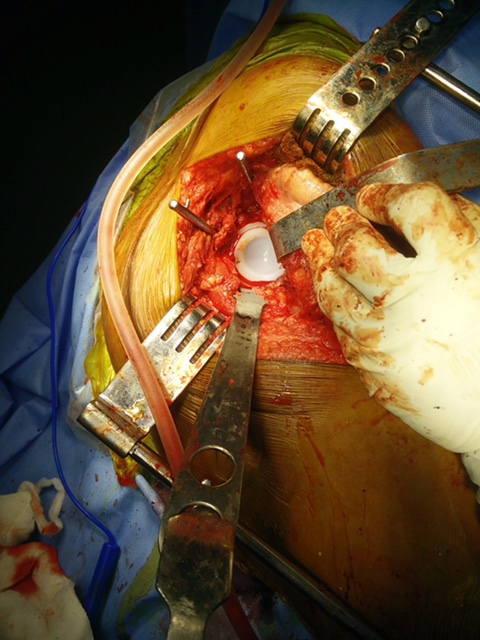
The extruded cement is trimmed with a knife and removed with a curette. Pressure is maintained till cement polymerizes. Look for and remove if any impinging osteophytes or cement projections are found.
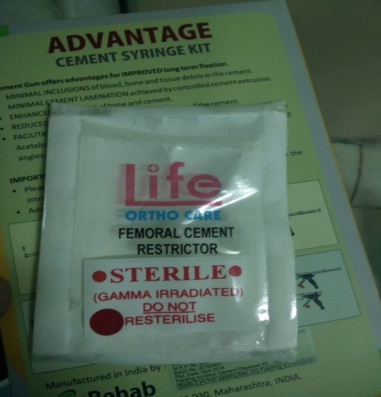
A cement restrictor is inserted 2-3cm below the level of the tip of the femoral prosthesis.
Canal is irrigated to remove loose debris, bone marrow and blood. Cavity is packed with hydrogen peroxide sponge. Drain tube is inserted on medial aspect of femoral neck. Cement is inserted into the cement gun and from there into the medullary canal.
Finally, the femoral component is inserted. Prosthesis is inserted in predetermined direction and anteversion.

The extruded cement is removed with knife or a curette. Hip is reduced after cement polymerizes. Closure is then done. Short external rotators are reattached using the ranawat sutures by making drill holes in posterior aspect of greater trochanter. Fascia, subcutaneous tissue and skin is sutured in layers. Drain is inserted.

Post-op Rehabilitation were given according to the following guidelines.
Ankle pumps, static quadriceps, isometric gluteal exercises were started immediately post op.
Patient was made to sit on the side of the bed on 2nd day and toe touch weight bearing with gait training was started by 5th post operative day.
Hip extension exercises were encouraged.
Observation and Result
Our study shows the most common age group amongst study population was 46 to 55 years (45%) followed by 56 to 65 years (25%). The mean age was 53.43 ± 10.45 years. There was higher number male patients (65%) as compared to female patients (35%). The most occupation amongst study population was Farmer (40%) followed by Housewife (15%) Worker (15%). The most common diagnosis amongst study population was Avascular necrosis (35%) followed by Rheumatoid arthritis (27.5%) and Ankylosing Spondylitis (15%). There was right side involvement in 65% and left side was involved in 35%. The most common type amongst study population was MOP (72.5%) followed by COP (27.5%). Our study demonstrated stem size of 3 (35.0%) was the most common stem size followed by stem size of 4 (32.5%) and stem size of 2 (27.5%). Superficial Infection (5.0%) was the most common complication followed by Dislocation (2.5%), DVT (2.5%) and foot drop (2.5%). The final outcome (Harris Hip Score) was good in 80% patients, 12.5% patients had fair and 7.5% patients had poor results. Our study shows in 34 to 45 years of age group fair and good outcome was observed in 14.3% and 85.7% respectively. In 46 to 55 years of age group fair, good and poor outcome was observed in 16.7%, 77.8% and 5.6% respectively. In 56 to 65 years fair, good and poor outcome was observed in 10%, 80% and 10% respectively. In 56 to 65 years of age group fair, good and poor outcome was observed in 10%, 80% and 10% respectively. More than 65 years of age group good and poor outcome was observed in 80% and 20% respectively. There was no significant difference in different age group and final outcome amongst study population. Our study shows in female patients fair, good outcome was observed in 7.1% and 92.9% respectively. In male patients fair, good and poor outcome was observed in 15.4%, 73.1% and 11.5% respectively. There was no significant difference in different sex and final outcome amongst study population. Our study shows in COP patients good outcome was observed in 100% while in MOP patients fair, good and poor outcome was observed in 17.2%, 72.4% and 10.3% respectively. There was no significant difference in type with final outcome amongst study population. Our study shows mean cup size, stem size, head size, pre-operative HHS and post-operative HHS was 53.43 ± 10.454 years, 45.68 ± 2.596, 2.85 ± 0.893, 29.90 ± 2.716, 51.25 ± 17.228, 79.33 ± 15.296 respectively.
| HIP 1 | PT 1 | 46 | M | FAR | OA | R | MOP | 47 | 3 | 32 | 47 | 92 | Nil | Good |
| HIP 2 | PT 2 | 57 | M | WOR | AVN | R | MOP | 47 | 3 | 32 | 77 | 97 | Nil | Good |
| HIP 3 | PT 2 | 57 | M | WOR | AVN | L | MOP | 47 | 3 | 32 | 7 7 | 97 | Nil | Good |
| HIP 4 | PT 3 | 48 | M | ENG | AVN | L | COP | 50 | 4 | 36 | 76 | 97 | Nil | Good |
| HIP 5 | PT 4 | 37 | F | HW | # NOF | R | COP | 43 | 2 | 28 | 11 | 87 | Nil | Good |
| HIP 6 | PT 5 | 62 | F | FAR | RA | L | MOP | 43 | 2 | 28 | 54 | 80 | Nil | Good |
| HIP 7 | PT 6 | 67 | M | RTD | AVN | R | MOP | 45 | 3 | 28 | 44 | 48 | Dislocation | Poor |
| HIP 8 | PT 7 | 49 | F | FAR | RA | L | MOP | 40 | 1 | 28 | 52 | 92 | Nil | Good |
| HIP 9 | PT 8 | 53 | M | FAR | AVN | R | COP | 45 | 3 | 28 | 60 | 87 | Nil | Good |
| HIP 10 | PT 9 | 55 | M | WOR | AVN | R | COP | 47 | 3 | 32 | 70 | 97 | Nil | Good |
| HIP 11 | PT 10 | 70 | F | HW | RA | L | MOP | 45 | 4 | 28 | 46 | 73 | Nil | Good |
| HIP 12 | PT 11 | 60 | F | HW | RA | R | MOP | 43 | 3 | 28 | 54 | 79 | Nil | Good |
| HIP 13 | PT 12 | 44 | M | DRI | AVN | R | COP | 53 | 4 | 36 | 72 | 98 | Nil | Good |
| HIP 14 | PT 12 | 44 | M | DRI | AVN | L | COP | 53 | 4 | 36 | 72 | 98 | Nil | Good |
| HIP 15 | PT 13 | 47 | M | DRI | AVN | L | COP | 47 | 3 | 32 | 80 | 98 | Nil | Good |
| HIP 16 | PT 14 | 53 | F | FAR | RA | R | MOP | 45 | 2 | 28 | 54 | 66 | Superficial infection | Fair |
| HIP 17 | PT 15 | 39 | M | FAR | AS | R | MOP | 47 | 2 | 28 | 46 | 58 | Nil | Fair |
| HIP 18 | PT 16 | 48 | M | POL | AVN | L | COP | 47 | 3 | 32 | 72 | 96 | Nil | Good |
| HIP 19 | PT 17 | 46 | M | FAR | AS | R | MOP | 45 | 4 | 28 | 30 | 41 | Nil | Fair |
| HIP 20 | PT 17 | 46 | M | FAR | AS | L | MOP | 45 | 4 | 28 | 30 | 41 | Nil | Fair |
| HIP 21 | PT 18 | 61 | M | FAR | AMR #NOF | R | MOP | 47 | 4 | 28 | 43 | 54 | Foot drop | Poor |
| HIP 22 | PT 19 | 48 | F | HW | RA | R | MOP | 40 | 2 | 28 | 60 | 84 | Nil | Good |
| HIP 23 | PT 20 | 50 | M | FAR | AS | L | MOP | 47 | 3 | 32 | 44 | 60 | Nil | Fair |
| HIP 24 | PT 21 | 53 | F | HW | RA | L | MOP | 43 | 2 | 28 | 50 | 78 | Nil | Good |
| HIP 25 | PT 22 | 51 | M | FAR | AVN | R | MOP | 45 | 2 | 28 | 62 | 70 | Dvt | Poor |
| HIP 26 | PT 22 | 51 | M | FAR | AVN | L | MOP | 43 | 2 | 28 | 62 | 70 | Dvt | Poor |
| HIP 27 | PT 23 | 63 | F | FAR | RA | L | MOP | 47 | 3 | 32 | 47 | 72 | Nil | Good |
| HIP 28 | PT 24 | 45 | M | WOR | # NOF | L | COP | 47 | 3 | 32 | 12 | 90 | Nil | Good |
| HIP 29 | PT 25 | 65 | M | WOR | OA | R | MOP | 45 | 2 | 28 | 63 | 93 | Nil | Good |
| HIP 30 | PT 25 | 65 | M | WOR | OA | L | MOP | 45 | 2 | 28 | 63 | 93 | Nil | Good |
| S.No. | PT No. | Age | Sex | Occ | Diag | Side | Type | Cup size | Stem size | Head size | Preop hhs | Postop hhs | Complication | Result |
| HIP 31 | PT 26 | 34 | M | DRI | AS | L | COP | 50 | 4 | 36 | 45 | 61 | Nil | Good |
| HIP 32 | PT 27 | 54 | F | FAR | AVN | L | MOP | 43 | 2 | 28 | 56 | 84 | Nil | Good |
| HIP 33 | PT 28 | 65 | M | WOR | AVN | R | MOP | 47 | 4 | 28 | 63 | 70 | Superficial infection | Fair |
| HIP 34 | PT 29 | 65 | M | WOR | AVN | R | MOP | 45 | 4 | 28 | 60 | 83 | Nil | Good |
| HIP 35 | PT 29 | 65 | M | WOR | AVN | L | MOP | 45 | 4 | 28 | 60 | 83 | Nil | Good |
| HIP 36 | PT 30 | 76 | M | RTD | OA | R | MOP | 47 | 4 | 28 | 52 | 78 | Nil | Good |
| HIP 37 | PT 31 | 46 | F | HW | RA | R | MOP | 45 | 2 | 28 | 54 | 87 | Nil | Good |
| HIP 38 | PT 32 | 47 | M | FAR | # NOF | R | MOP | 47 | 3 | 32 | 14 | 97 | Nil | Good |
| HIP 39 | PT 33 | 48 | M | FAR | AS | R | COP | 50 | 4 | 36 | 37 | 56 | Nil | Good |
| HIP 40 | PT 33 | 48 | M | FAR | AS | L | COP | 53 | 4 | 36 | 37 | 56 | Nil | Good |
| HIP 41 | PT 34 | 37 | F | FAR | # NOF | L | MOP | 45 | 2 | 28 | 11 | 94 | Nil | Good |
| HIP 42 | PT 35 | 68 | F | HW | RA | R | MOP | 43 | 2 | 28 | 53 | 76 | Nil | Good |
| HIP 43 | PT 35 | 68 | F | HW | RA | L | MOP | 43 | 2 | 28 | 53 | 76 | Nil | Good |
| HIP 44 | PT 36 | 57 | M | POL | AVN | L | MOP | 43 | 2 | 28 | 69 | 88 | Nil | Good |
| HIP 45 | PT 37 | 75 | M | RTD | OA | R | MOP | 45 | 3 | 28 | 56 | 79 | Nil | Good |
| HIP 46 | PT 38 | 59 | M | SK | AVN | R | MOP | 47 | 3 | 32 | 58 | 94 | Nil | Good |
| HIP 47 | PT 38 | 59 | M | SK | AVN | L | MOP | 47 | 3 | 32 | 58 | 94 | Nil | Good |
| HIP 48 | PT 39 | 40 | M | POL | AS | R | COP | 47 | 4 | 32 | 43 | 63 | Nil | Good |
| HIP 49 | PT 40 | 49 | F | FAR | RA | R | MOP | 43 | 1 | 28 | 53 | 76 | Nil | Good |
Discussion
Total hip replacement (THR) is one of the most successful orthopaedic interventions,[12] and is the recommended treatment for hip arthritis.[13], [14] Majority of the total hip arthroplasties are carried out in patients suffering from osteoathritis.[15], [16], [17], [18] The remaining diagnoses for elective THR included avascular necrosis (3.7%), dysplasia (1.3%) and rheumatoid arthritis (1.3%) and for TKR; rheumatoid arthritis (1.7%), inflammatory arthritis (0.5%) and necrosis (0.4%).[15] However, published reports suggest considerable variability in outcomes and revision rates even within groups implanted with the same prosthesis and within the same institution. A considerable body of work has explored the factors related to implant and procedure that influence outcome after THR, sometimes in long term studies involving the analysis of some 200000 implant procedures.[12], [19] Although these investigations have successfully identified a number of important variables related to implant, cement, procedure, surgeon and others that influence an outcome usually expressed as “implant survival”, patient related factors other than age or sex that influence outcome after THR have received comparatively little attention.
Newest advances in cementing techniques, the Charnley low friction cemented arthroplasty is regarded by many as the standard treatment for comparison purposes for THR.[20], [21], [22] Whereas it is generally believed that the cemented femoral component provides an immediate post-operative advantage (i.e., of intimate contact between the prosthesis cement and the bone, which permits dramatic early relief of pain and more weight bearing), there is divided opinion over long-term results.
The surgery was performed through an incision over the posterior part of the greater trochanter through the fascia, followed by blunt dissection of gluteus maximus. The external rotators were detached and the hip capsule incised.[23] The hip was dislocated by internal rotation and flexion. During closure of the wound, the capsule was repaired and the external rotators were re-inserted using a heavy absorbable suture.
Surgical approach for total hip replacement has remained controversial.[24], [25], [26] Posterior approach is known to give less blood loss, to shorten operation time and to allow optimal component positioning.[27], [11] It is considered an easy access, with less soft tissue dissection than other hip approaches, especially direct lateral, and is associated with fewer gait problems as well.[24] However, a higher percentage of posterior dislocation (3.2% to 4.2%) of the implanted hip has been observed with the posterior approach.[26], [25] Nevertheless, reattachment of the posterior capsular flap and tendons (of piriformis and obturator internus) to the greater trochanter have reduced the incidence of dislocation[28], [29] from 4.8% to 0.7% in two groups of patients without and with posterior capsular repair respectively.[30] Further, most dislocations happen to be posterior and a majority occur within the first six months of implantation.[28]
The strength of this study is that all hips were primary total arthroplasties although there was 1 revision of previously done hemiarthroplasty none were revision total hip arthroplasties, all were done using a uniform technique, done by same surgeon and no patient lost for follow - up. The limitation of the study is that the sample size is less and the follow-up duration is not very long so as to demonstrate the long term complications of this procedure.
Findings of this study and comparison with other studies
Age group
In the present study, the most common age group amongst study population was 46 to 55 years (45%) followed by 56 to 65 years (25%). The mean age was 53.43 ± 10.45 years. Similarly in the study conducted by A.T. Shanmugaraja et al.,[31] 8 out of 15 patients were in the age group of 50-60 years, five were in the age group of 40-50 years, one each were in the age group of 30-40 years, and 20-30 years age group. In western literature, as per Harkness,[32] Eftekhar,[33] Charney[34] total hip arthroplasty has primarily been described for patients in older age group of sixty and above. In study conducted by A. Chandra Sekhar et al.,[35] all patients were found to be in the 50 and above age group, with age ranging from 50 to 85 years and a mean age of 59.68 years.
Sex predilection
In the present study, there was higher number male patients (65%) as compared to female patients (35%). This was in agreement to study conducted by A. Chandra Sekhar et al.[35] Majority, 17 (68%) were males and 8 (32%) were females. On the contrary, S. Zimmerrnan et al.[36] observed higher number of female population (63.8%).
Occupation
In the present study, the most common occupation undergoing THR amongst study population was Farmer (40%) followed by Housewife (15%) Worker (15%).
Diagnosis
In the present study, the most common diagnosis amongst study population was Avascular necrosis (35%) followed by Rheumatoid arthritis (27.5%) and AS (15%). Similarly in the study conducted by A.T. Shanmugaraja et al.,[31] 10 (67%) patients were diagnosed as Secondary Arthritis due to Avascular Necrosis, four as primary Osteoarthritis (26%) and one as Rheumatoid Arthritis (7%).
Side involvement
In the present study, there was right side involvement in 65% and left side was involved in 35%.
Complications
In the present study, superficial Infection (5.0%) was the most common complication followed by Dislocation (2.5%), DVT (2.5%) and Foot Drop (2.5%). This was is agreement with the study conducted by Kuldip Salgotra et al.,[37] in which the infection (2 out of 92 cases) and Dislocation (3 out of 92 cases) were the common complications. Fackler CD et al.[38] in their study have reported a 2% incidence of dislocation after primary hip arthroplasty.
Final outcome (Harris Hip Score)
In the present study, Final outcome (Harris Hip Score) was good in 80% patients, 12.5% patients had Fair and 7.5% patients had poor results. Similarly in the study conducted by Chandra Sekhar et al.,[27] 2015, (84%) had excellent results, 2 (8%) had good result and 2 (8%) had fair results. Study conducted by A.T. Shanmugaraja et al.,[31] reported 73% had excellent outcome and 27% had good outcome after THR. Similarly in the study conducted by Bangabandhu Sheikh et al.,[39] 76.2% patients had excellent, 19.1% had good and 4.8% had fair outcome after THR. The post op Harris Hip Score observed in our study is comparable to that in the study conducted by Garino and Steinberg[40] who reported increase in the Harris Hip Score from 45 pre operatively to 92 in the post op period.
Kavanagh et al.[41] (1989) conducted a study in 170 out of the 333 operated cases of Charnley THR over 15 years. It was noted that excellent or good results were noted in 78% of the hips. Schulte et al. [42] (1993) conducted a study in 322 hips out of 330 operated hips in a 2 year period between July 1970 and April 1972 and followed up for a period of 20 years. Out of the 98 hips in 83 living patients, 83 (85%) hips had no pain whereas 14 (14%) had mild pain and 1 (1%) moderate pain. Thus the outcome is comparable with the long term studies conducted by Kavanagh[41] et al. and Schulte[42] et al. although long term follow up is required in our study for assessment of late complications.
In the present study, in 34 to 45 years of age group fair and good outcome was observed in 14.3% and 85.7% respectively. In 46 to 55 years of age group fair, good and poor outcome was observed in 16.7%, 77.8% and 5.6% respectively. In 56 to 65 years fair, good and poor outcome was observed in 10%, 80% and 10% respectively. In 56 to 65 years of age group fair, good and poor outcome was observed in 10%, 80% and 10% respectively. In more than 65 years of age group good and poor outcome was observed in 80% and 20% respectively. There was no significant difference in different age group and final outcome amongst study population.
In the present study, in female patients fair and good outcome was observed in 7.1% and 92.9% respectively. In male patients fair, good and poor outcome was observed in 15.4%, 73.1% and 11.5% respectively. There was no significant difference in different sex and final outcome amongst study population.
Source of Funding
None.
Conflict of Interest
None.
Conclusion
Based on our experience and results, we conclude that cemented total hip replacement is an excellent procedure in the management of diseased and destroyed hips with chronic and incapacitating pain in elderly patients.
Secondary osteoarthritis of the hip due to avascular necrosis of the femoral head is the most common cause of chronic hip pathology.
Cemented total hip replacement is the procedure of choice in elderly patients.
Conservative management with analgesics is not acceptable.
Cemented total hip replacement is a cost-effective procedure.
The assessment of clinical results of cemented total hip replacement has shown that there is definitive improvement with regard to pain, function and range of motion post-operatively.
With proper patient selection, adequate planning, armamentarium, meticulous surgical technique, we have achieved results comparable to other authors. In a nutshell, in our institute, this procedure done with utmost technical precision has provided us very good clinical results.
Moore’s approach is a safe and effective approach for total hip replacement
Long term studies are necessary to study the late complications and to prove the efficacy of the implants and procedure.
References
- M L Parker, G Pryor, K Gurusamy. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomized controlled trial in 400 patients. J Bone Joint Surg Br 2010. [Google Scholar]
- R Blomfeld, H Tornkivist, K Eriksson. A Randomized control trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in the elderly patients. J Bone Joint Surg Br 2007. [Google Scholar]
- J F Keating. . Femoral Neck Fractures. Rockwood and Greens fracture in adults 2015. [Google Scholar]
- C. Hopley, D. Stengel, A. Ekkernkamp, M. Wich. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ 2010. [Google Scholar] [Crossref]
- . Scottish Intercollegiate Guidelines Network. Management of Hip Fracture in Older People. Edinburgh: SIGN. 2009. [Google Scholar]
- Anshul Dahuja. A Prospective Study on Role of Cemented Total Hip Arthroplasty in Osteonecrosis of Hip Joint with Femoral Head Collapse in Elderly: A Study of 100 Cases. IOSR J Dent Med Sci 2013. [Google Scholar]
- M A Mont, D S Hungerford. Current concept review, Non- traumatic avascular necrosis of the femoral head. J Bone Joint Surg 1995. [Google Scholar]
- P Gregg. National Total Hip Replacement Outcome Study. . [Google Scholar]
- J W Harkess, J Crockarell. . Arthroplasty of the Hip. Campbells operative orthopaedics 2013. [Google Scholar]
- R Robinson, H Robinson, E Salvati. A comparison of the transtrochanteric and posterior surgical approaches for total hip replacement. Clin Orthop 1980. [Google Scholar]
- A J Vicar, C R Coleman. A comparison of the anterolateral, transtrochanteric and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop Relat Res 1984. [Google Scholar]
- Peter Herberts, Henrik Malchau. Long-term registration has improved the quality of hip replacement: A review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand 2000. [Google Scholar]
- Acr. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000. [Google Scholar]
- A Pendleton, N Arden, M Dougados, M Doherty, B Bannwarth, J W Bijlsma. EULAR recommendations for the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2000. [Google Scholar]
- . Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide. 2011. [Google Scholar]
- . Swedish Hip Arthroplasty Register. Annual Report 2010 Göteborg. . [Google Scholar]
- . The Swedish Knee Arthroplasty Register. Annual Report 2010 Lund, 2011. . [Google Scholar]
- . National Joint Replacement Registry for England and Wales. 8th Annual Report 2011 Hertfordshire, 2011. . [Google Scholar]
- S J Birtwistle, K Wilson, M L Porter. Long-term survival analysis of total hip replacement. Ann R Coll Surg Engl 1996. [Google Scholar]
- Mark A. Mehlhoff, Clement B. Sledge. Comparison of cemented and cementless hip and knee replacements. Arthritis Rheumatism 1990. [Google Scholar]
- R D Mulroy, W H Harris. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg 1990. [Google Scholar]
- J Older, R Butorac. Charnley low friction arthroplasty (LFA). J Bone Joint Surg 1992. [Google Scholar]
- S Hoppenfeld, P Deboer, R Buckley. . Surgical Exposures in Orthopaedics: The Anatomic Approach 2009. [Google Scholar]
- B M Jolles, E R Bogoch. Surgical approach for total hip arthroplasty: direct lateral or posterior?. J Rheumatol 2004. [Google Scholar]
- Merrill A. Ritter, Leesa D. Harty, Michael E. Keating, Philip M. Faris, John B. Meding. A Clinical Comparison of the Anterolateral and Posterolateral Approaches to the Hip. Clin Orthop Relat Res 2001. [Google Scholar]
- John L. Masonis, Robert B. Bourne. Surgical Approach, Abductor Function, and Total Hip Arthroplasty Dislocation. Clin Orthop Relat Res 2002. [Google Scholar]
- A. W. ElMaraghy, E. H. Schemitsch, J. P. Waddell. Greater Trochanteric Blood Flow During Total Hip Arthroplasty Using a Posterior Approach. Clin Orthop Relat Res 1999. [Google Scholar]
- G. M. J. van Stralen, P. J. Struben, C. J. M. van Loon. The incidence of dislocation after primary total hip arthroplasty using posterior approach with posterior soft-tissue repair. Arch Orthop Trauma Surg 2003. [Google Scholar]
- Steven H Weeden, Wayne G Paprosky, Jack W Bowling. The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty 2003. [Google Scholar]
- Richard E. White, Timothy J. Forness, James K. Allman, Daniel W. Junick. Effect of Posterior Capsular Repair on Early Dislocation in Primary Total Hip Replacement. Clin Orthop Relat Res 2001. [Google Scholar]
- A T Shanmugaraja, R Neelakrishnan, V Barathiselvan, D Dhiviyaraj. Functional And Clinical Outcomes Of Total Hip Arthroplasty In Arthritis Hip. Int J Modn Res Revs 2015. [Google Scholar]
- J W Harkess, J R Crockarell, S T Canale, J H Beaty. Arthroplasty of the Hip. Campbell’s Operative Orthopaedics 2008. [Google Scholar]
- N S Eftekhar. Total hip replacement using principles of low-friction arthroplasty: The Hip. CM Evarts (ed) Surgery of the musculoskeletal system 1983. [Google Scholar]
- J Charnley. . Low friction arthroplasty of the hip: Theory and practice 1979. [Google Scholar]
- C Sekhar, A Mittal, R Rallapalli, R Biju, Prasad Sy. Evaluation and Outcome of Total Hip Replacement in Adults with Arthritis. J Dent Med Sci (IOSR-JDMS) 2015. [Google Scholar]
- S Zimmerman, W G Hawkes, J I Hudson. Outcomes of surgical management of total hip replacement in patients aged 65 years and older: cemented versus cementless femoral components and lateral or anterolateral versus posterior anatomical approach. J Orthop Res 2012. [Google Scholar]
- R Kuldip, Salgotra. Cemented Total Hip arthroplasty: A study of 100 cases. MGM J Med Sci 2016. [Google Scholar]
- C D Fackler, R Poss. Dislocation in Total Hip Arthroplasties. Clin Orthop Relat Res 1980. [Google Scholar]
- J P Garino, M E Steenberg. Total Hip Arthroplasty in Patients with Avascular Necrosis of the Femoral Head; A 2??? to 10-Year Followup. Clin Orthop Relat Res 1997. [Google Scholar]
- B F Kavanagh, M A Dewitz, D M Ilstrup, R N Stauffer, M B Coventry. Charnley total hip arthroplasty with cement. Fifteen-year results.. J Bone Jt Surg 1989. [Google Scholar]
- K R Schulte, J J Callaghan, S S Kelley, R C Johnston. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up. The results of one surgeon.. J Bone Jt Surg 1993. [Google Scholar]
How to Cite This Article
Vancouver
Modi R, Thipse J. Study on outcome of cemented total hip replacement by posterolateral approach to hip [Internet]. Indian J Orthop Surg. 2025 [cited 2025 Sep 09];6(2):58-68. Available from: https://doi.org/10.18231/j.ijos.2020.012
APA
Modi, R., Thipse, J. (2025). Study on outcome of cemented total hip replacement by posterolateral approach to hip. Indian J Orthop Surg, 6(2), 58-68. https://doi.org/10.18231/j.ijos.2020.012
MLA
Modi, Rahul, Thipse, Jayant. "Study on outcome of cemented total hip replacement by posterolateral approach to hip." Indian J Orthop Surg, vol. 6, no. 2, 2025, pp. 58-68. https://doi.org/10.18231/j.ijos.2020.012
Chicago
Modi, R., Thipse, J.. "Study on outcome of cemented total hip replacement by posterolateral approach to hip." Indian J Orthop Surg 6, no. 2 (2025): 58-68. https://doi.org/10.18231/j.ijos.2020.012
