- Visibility 10 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijos.2020.018
-
CrossMark
- Citation
Functional outcome of scaphoid nonunion treated with herbert screw and bone grafting
- Author Details:
-
Bibin K Baby *
-
Jyothish K
-
Aju T Thomas
Introduction
Scaphoid fractures are common in young active individuals and its management is controversial in various occasions. The main treatment modalities include scaphoid cast immobilization, percutaneous k wire fixation, bone grafting techniques with immobilization and Herbert screw fixation with or without bone grafting.[1] These fractures frequently result in nonunion either due to treatment problems or due to failure in identifying the fractures in initial radiographs. Xrays of the scaphoid are very difficult to interpret, and even if the fracture appears to be united after initial treatment, radiographic follow-up later shows the development of established nonunion in many cases. Many studies suggest that the real incidence of non-union after conservative treatment of scaphoid is of the order of fifty percentage.[2], [3]
The symptomatic nonunion of the scaphoid is really a disabling condition. Another important concern is that the majority of patients are young working-class group and hence surgical intervention in these nonunion cases are very important especially for making them return to their jobs.
In this study we evaluated 12 patients with established nonunion of scaphoid treated with Herbert screw fixation and cancellous bone grafting. The functional outcome was evaluated with modified Mayo wrist score.[4] Herbert screw fixation gives enough stability to allow healing of the scaphoid nonunion without additional plaster immobilization and bone grafting aids structural integrity by correcting deformity and promotes bone healing.
Materials and Methods
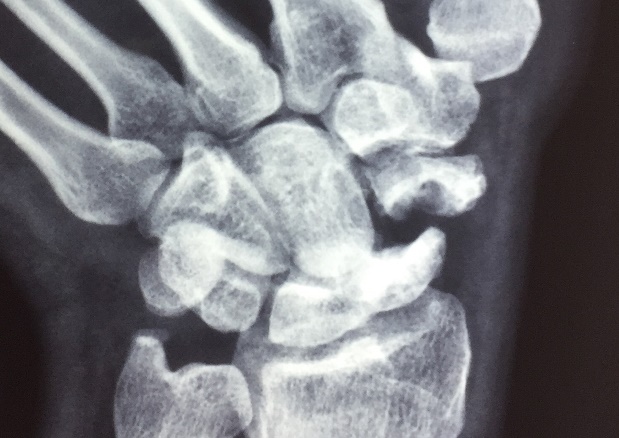
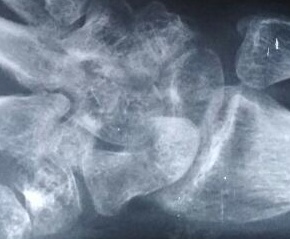
The study was conducted over a period from December 2017 to May 2018 in The Department of Orthopedics, Government Medical College, Thrissur. All the cases were referrals from peripheral centers with a possible diagnosis of scaphoid nonunion after failed conservative treatment. All the patients were initially assessed with fresh radiographs and MRI wrist was taken in all cases. The injuries were classified according to Herbert’s Classification. One patient was excluded from the study due to severe secondary osteoarthritic changes which made him unsuitable for this procedure.
During initial assessment in the OPD the mode of injury, previous treatment, current symptoms and disability in job and daily activities were recorded. Clinical examination included the assessment of tenderness, active and passive range of movement in wrist, and grip strengths were also measured. AP, Lateral and oblique view radiographs of wrist were taken preoperatively, the same technique also being used at follow-up examinations. MRI was taken for assessing the fracture morphology and classification of the fracture properly. The diagnosis of radiological union required clear evidence of bony trabeculae transversing the graft from proximal to the distal pole in standard scaphoid views.

Reconstruction of nonunion (type D) was advised for all symptomatic cases and all consenting patients irrespective of the age group and were included in the study. Patients with associated neurovascular injuries, other carpal bone fracture of same limb, those with previous surgery of fractured area and those with musculoskeletal diseases are also excluded from the study. Surgery was not performed for patients with advanced radiocarpal osteoarthritis or in asymptomatic patients.
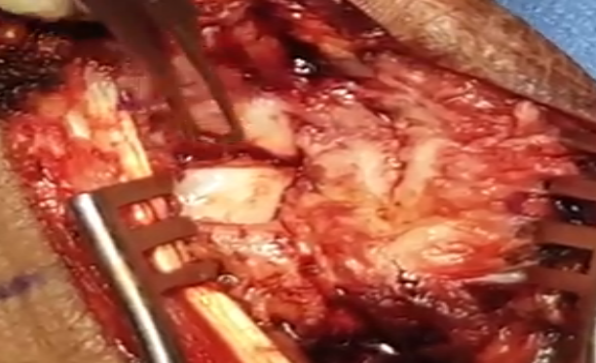
A standard volar approach was used for internal fixation in all cases. The state of the articular cartilage and synovium, the presence of any fibrous adhesions or interposition at the fracture site was assessed intraoperatively. The condition of the fracture surfaces and degrees of fracture mobility were carefully assessed and the fracture site was observed for bleeding after freshening. For type D1 non unions, the synovial adhesions and fibrous tissues were meticulously removed without destabilizing the fracture, and cancellous graft was used to fill any defects after curetting out all the avascular tissue and cysts. All types D2 cases, the pseudarthroses was removed from fracture surfaces and were then reconstructed using a corticocancellous bone graft. The Herbert screw was then inserted freehand, using the drill guide wire. Most bone grafts were taken from the contralateral iliac crest or from the distal radius depending upon the amount of graft needed and size of the nonunion gap.


A firm padded removable splints were used to support the wrist for the first two weeks and after the suture removal, patients are advised to start mobilizing exercises of the wrist. During the initial eight weeks after surgery, patients were advised to avoid excessive loading of their wrist and to avoid contact sports. Light removable splints were prescribed only when the patient was unlikely or unwilling to comply with this advice.
Patients were asked to attend for routine review at 3weeks, 6weeks, 9 weeks and3 months and any additional visits being scheduled as required. Standard wrist radiographs were taken at each visit and a detailed clinical assessment was recorded. All assessments and radiographs were reviewed by principal investigator, who analyzed the clinical results using modified Mayo s wrist score. Radiographically fractures were recorded as united only if cross-trabeculation was present and the fracture line was no longer visible on any of the standard views. But our study duration is inadequate comment on radiological outcome analysis and hence it was not included in the main study results.
Results
There were 12 cases of scaphoid nonunion treated with Herbert screw fixation and cancellous bone grafting. All the patients were males and dominant hand was involved in 10 cases. Out of 12 patients five patients had road traffic accidents, six had fall on outstretched hand and one fracture caused by assault. The right wrist was affected in 9 cases and left in three patients.
The mean time from injury to surgical fixation was 13 months. The mean age of the patients was 27.9 years. The occupations of the patients in terms of weight loading of the wrist were heavy loading in 6 patients, light loading in 2 patients and clerical work in 4 patients. Since all the patients were referral cases with nonunion, they were initially been treated in plaster of Paris for an average of 13 months.


All the twelve patients were regularly followed up and was evaluated for clinical and radiological outcomes. Our study was mainly focusing on the short-term functional outcome of the patient rather than radiological outcome. Our series resulted in 58.3% excellent, 33.3% good and 8.3% fair functional outcomes. one patient each in good and fair groups had mild pain post operatively. 91% of patients were satisfied with the outcome of the procedure mostly because they could return to job with a painless joint.

Wrist function was assessed by range of movement and grip strength which was greatly improved after herbert screw fixation of the scaphoid. The movement which was mostly difficult improve was wrist dorsiflexion after reconstruction. The rigid internal fixation of the scaphoid resulted in significant decrease in pain. Most of our patients had moderate to severe pain preoperatively, but 83.3% cases had no pain at the latest review.


Based on our study results we like to propose that the successful internal fixation of scaphoid with Herbert screw and bone grafting can improve the wrist function considerably. The preoperative incidence of arthritis of wrist had not significantly worsened on post-operative follow ups.
The most common complication of surgery was the postoperative pain and discomfort at the donor site in case of the bone graft taken from iliac crest, although this resolved with time. One superficial wound infection resolved completely with antibiotic therapy only. None of the wrists had protrusion of the screw or developed nonunion. One of the patients had early signs of sudeks sympathetic dystrophy (RSD) after surgery.
Discussion
The main purpose of this study was to evaluate the short-term functional outcome after internal fixation of scaphoid non unions using Herbert screw and bone grafting in those cases initially treated with conservative techniques. Many studies in the literature shows satisfactory outcome after conservative treatment, but the actual incidence of non-union with conventional treatments appears considerably high.[2], [3], [5] The morbidity associated with prolonged use of plaster immobilization is also very concerning especially in young individuals.
Even though union can be achieved in majority of cases,[6] long periods of immobilization may be needed. If conservative management fails, then the Matti-Russe procedure may be effective in 85% of cases.[7], [8] But this procedure also will not reduce the period of immobilization. In a study Dias, Brenkel and Finlay[9] reviewed 82 patients treated conservatively after almost two years: and concluded that ten patients had definite nonunion and another 20 cases had a visible fracture line.
But conservative management of fracture scaphoid with cast is still a common treatment modality, but it results in unacceptably high rate of nonunion and associated poor functional outcomes. Hence for displaced scaphoid fracture and for non-unions, open reduction and internal fixation will be the ideal modality of management.[10]
Our study shows that internal fixation using the Herbert bone screw and bone grafting in scaphoid nonunion results in early symptomatic relief and faster functional recovery. It also shows that the screw gives sufficient structural stability to allow normal function of the wrist. The fixation remains stable enough to allow revascularization of the bone. We also encourage early normal use of the wrist by avoiding plaster immobilization postoperatively. This aids in rapid functional improvement of wrist and also reduces the development of stiffness of joint and osteoporosis. We strongly support early postoperative wrist mobilization and condemn the use of plaster after Herbert screw fixation. The results of our study confirm that internal fixation with herbert screw along with bone grafting leads to better results than other standard techniques mainly due to the accuracy of scaphoid reconstruction and the benefits of early postoperative rehabilitation. We therefore strongly recommend that internal fixation with bone grafting for scaphoid nonunion, even in cases with ischemic nonunion.
In our series the patients are of young working class with a mean age group was 27.9 years and they cannot afford to stay off from job for the two to four months often required after bone grafting surgery alone. One of the important advantages of internal fixation is that it permits an early return to normal job especially in the scenario of more young individuals presenting with nonunion.
According to Alexandros E Beris et al.[11] Herbert screw along with iliac wedge graft was more effective for correcting the bony deformity and gives improved stabilization. They also suggested that the long periods of postoperative immobilization will negatively affect the postoperative wrist function. D. O. Ferguson, V. Shanbhag et al.,[12] in their systematic review assesses outcomes of 5464 scaphoid non-union outcomes within the 144 studies treated with bone graft surgery for scaphoid fracture non-union, reported that the union rates for vascularized and non-vascularized bone graft were 84% and 80%, respectively.
S Eggli, D.L Fernandez et al.[4] conducted a retrospective review of thirty seven patients with scaphoid nonunions treated by bone grafting and internal fixation with an mean follow-up period of 5.7 years. Their study concluded that, fifteen patients had an excellent result, eleven had a good result, four had a fair result and seven had a poor result.
According to Merrell G.A., Wolfe S.W., et al.[13] who done a systematic meta-analysis of the literature on the treatment of scaphoid nonunion which included 36 articles, for the unstable nonunion, screw fixation with grafting produces 94% union rate compared to K-wires and wedge grafting (77% union). They also suggested that there is no evidence supporting the postoperative immobilization after solid screw fixation.
Yi-Chao Huang, Yih Liu et al.[14] retrospectively reviewed 49 patients treated with Herbert’s screw fixation and bone graft and got a union rate of 93.9% with 59% excellent results and 35% good results.
In our study series we encountered a case of superficial wound infection and one patient had reflex sympathetic dystrophy. This is in consistent with other studies in the literature. The main disadvantage of our study was the small study group and relatively small study period. But since we are analyzing the early functional recovery and short-term outcomes of the patients, the follow up period is justified.
The bone grafting and Herbert’s screw fixation is definitely a reliable modality of treatment which gives satisfactory functional outcome. The important factor is the postoperative immobilization and we support early mobilization of wrist and condemn the use of any plaster splints. We recommend this modality of treatment for all scaphoid non union cases without significant degenerative arthritis of wrist joint.
Conclusions
Our study concluded that the management of scaphoid non unions with the Herbert screw and bone grafting can provide enough stability to allow fracture healing without much external splintage. The healing of the nonunion is better than that in other surgeries like k wire fixation or bone graft surgeries alone. Wrist function recovers much quicker after rigid internal fixation and early post-operative mobilization. Most of the patients will return to jobs very early with a pain free joint and the incidence of complications is low in this modality of treatment.
Source of Funding
None.
Conflict of Interest
None
References
- Charles M Court -Brown, J D Heckman. . Rockwood and Green Fractures in Adults 2015. [Google Scholar]
- S. L. Filan, T. J. Herbert. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg 1996. [Google Scholar]
- T J Herbert, W E Fisher. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg 1984. [Google Scholar]
- S. Eggli, D. L. Fernandez, T. Beck. Unstable Scaphoid Fracture Nonunion: A Medium-Term Study of Anterior Wedge Grafting Procedures. J Hand Surg 2002. [Google Scholar]
- P J. Radford, M. H. Matthewson, B. F. Meggitt. The Herbert Screw for Delayed and Non-Union of Scaphoid Fractures: A Review of Fifty Cases. J Hand Surg 1990. [Google Scholar]
- W P Cooney, J H Dobyns, R L Linschield. Fractures of the scaphoid: a rational approach to management”. Clin Orthop 1980. [Google Scholar]
- B. J. Dooley. Inlay bone grafting for non-union of the scaphoid bone by anterior approach. J Bone Joint 1968. [Google Scholar]
- Emanuel Trojan. Grafting of Ununited Fractures of the Scaphoid. Proc R Soc Med 1974. [Google Scholar]
- J J Dias, I J Brenkel, D B Finlay. Patterns of union in fractures of the waist of the scaphoid. J Bone Joint Surg 1989. [Google Scholar]
- V K Mittal. Conservative management of fracture scaphoid. Indian J Orthop 2006. [Google Scholar]
- Alexandros E Beris, Panayotis N Soucacos, Theodore Xenakis, Konstantinos Malizos, Gregoris Mitsionis, Socratis Varitimidis. Scaphoid nonunion treated with bone graft and Herbert screw. Acta Orthop Scand 1997. [Google Scholar]
- D. O. Ferguson, V. Shanbhag, H. Hedley, I. Reichert, S. Lipscombe, T. R. C. Davis. Scaphoid fracture non-union: a systematic review of surgical treatment using bone graft. J Hand Surg 2016. [Google Scholar]
- Gregory A. Merrell, Scott W. Wolfe, Joseph F. Slade. Treatment of scaphoid nonunions: Quantitative meta-analysis of the literature. J Hand Surg 2002. [Google Scholar]
- Yi-Chao Huang, Yih Liu, Tain-Hsiung Chen. Long-term results of scaphoid nonunion treated by intercalated bone grafting and Herbert’s screw fixation—a study of 49 patients for at least five years. Int Orthop 2009. [Google Scholar]
