Introduction
Surgical fixation with plating is the standard treatment for displaced forearm fracture. Radius is traditionally approached by Henry’s volar approach1 and Thomson’s dorsal approach.2 Volar approach is needs exposure of radial artery and dorsal approach requires exposure of posterior interossious nerve respectively. Exposure of these vital structures fand preservation is associated with some complication and time consuming.3 The radius has a lateral bow which makes the application of plate on volar or dorsal surface difficult. Maintaining adequate radial bow and interossueous space is important for good functional outcome.
A novel lateral approach was described by Muhammed Hanif et al4 in 2014. This approach utilizes t he plane between ECRL and brachioradialis (BR). It is devoid of any major neurovascular structure and the plate can be applied on lateral tensile surface of radius. However, Backiaraj Devaraj et al6 in their cadaver based study suggested the plane between ECRL and ECRB for proximal and plane between the ECRL and BR for distal shaft of radius respectively. In this study we wanted evaluate the clinical and radiological outcome of modified direct lateral approach to radius.
Materials and Methods
This retrospective study was conducted in the Dhanalakshmi Srinivasan Medical College, Perambalur, Tamilnadu, India. Patients with Fracture of both bone forearm and isolated fracture of radius, who underwent radial fixation using modified lateral approach, were included in the study. Patients with neurovascular injury, open fracture, bilateral fracture, more than five days old fracture and patient who had previous history of trauma and immobilization of either upper limb were excluded from this study.
Preoperative evaluation includes routine musculoskeletal examination with more focus on radial pulse, muscles supplied by PIN and sensation in dorsum of hand. Anteroposterior and lateral radiographs of forearm were obtained to evaluate fracture carecteristics. The Active range of motion (ROM) of contralateral forearm and wrist were recorded by physiotherapist.
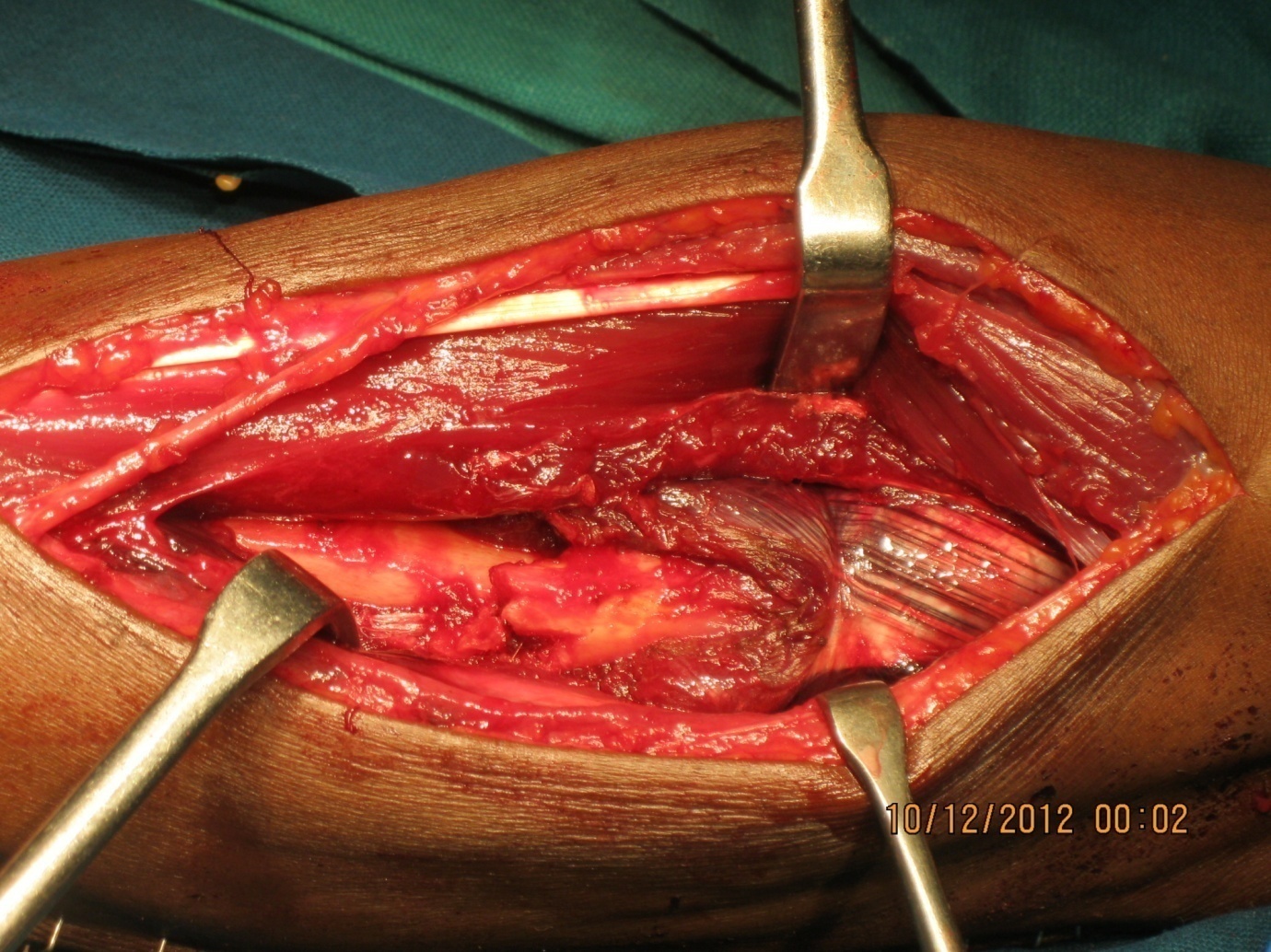
All the surgeries were done by single surgeon. Surgery was done under regional block and tourniquet. Patient is supine with forearm on arm board in mid prone position. Tourniquet was used in radius fixation and the ulna fixation done without tourniquet. Skin incision centered over the radial fracture along a line which is drawn from a lateral epicondyle to radial styloid. Subcutaneous tissue and facia incised along the skin incision. Branches of antebrachial cutaneus nerve in the proximal part to be identified and preserved. ECRL was identified by its relatively short muscle belly and long tendon (Figure 1). The plane between ECRL and ECRB is identified and retracted. Flexion of elbow to relaxes the ECRL aids in retraction. This will expose the whole lenth of diaphysis with supinator in proximal third (Figure 2), PT in middle third and distal third lateral suface is free from any muscle attachment but it is crossed by tendons of Abductor policis longus(APL) and Extensor policis brevis(EPB). Pronator teres insertion is not disturbed and the plate applied over its insertion. For distal fracture the tendons of APB and EPL retracted dorsaly or the plate may be glided underneath the tendons. The plate is applied on lateral surface and the radial bow is maintained by pre-contouring the plate using a template. Ulna is fixed using posterior approach. Fixation both ulna and radius (Figure 3) was done using a 3.5 mm limited contact dynamic compression plate (LC-DCP) or dynamic compression plate (DCP).
Mobilisation started on first post op day as tolerated by the patient under the direction of a physical therapist. ROM advanced incrementally as fracture site healing progressed, with a goal of full ROM by three weeks. Postoperative evaluation included clinical and radiographic evaluation at three, six, nine and twelve months. Clinical evaluation focused on measurement of ROM (forearm and wrist) by physiotherapist.
The postoperative radiographs included biplanar views of forearm, which were evaluated for progression of healing. Healing was assessed by disappearance of fracture line and bridging callus formation.
Table 1
Clinical results at 12 months follow up
Results
Between May 2016 and August 2018, twenty patients (13 male patients and seven female patients) underwent ORIF of radius using modified lateral approach. Of which 16 patients had both bone forearm fracture and 4 had isolated radius fracture. The average age at the time of the procedure was 34 years (range 16 to 64 years). 12 patients had involvement of right forearm and eight on left forearm. The average duration of time since injury to surgery is 2.4 days (ranging from one to five days). Average tourniquet time for radius fixation using lateral approach was 32 minutes (range from 25 to 50 minutes).
All ulna fracture and all but one radius fracture were united at six months post op. One radius went for delayed union and united at 9 months follow up (Figure 4). Fracture union rate is 100% at one year in our study. At one year follow up (Table 1) arc of forearm rotation was 142.30 (90.8% compared to normal side) and arc of wrist motion was 142.80 (94.5% compared to normal side).
Discussion
There are very few studies on lateral approach to radius5 and lateral platting of radius.5 Most of the studies used either volar approach with volar plating or dorsal approach with dorsal plating.
Average rate of union in our study is 100%, compared to 94.73% by Muhammad Haseeb et al,5 90% by Chapman et al,6 98% by Anderson et al7 and 97% by Hadden et al.8
The increased union rate in our study may be due less vascular insult with this approach or may be due to small sample size. We do not erase any muscle from bone for application of plate in this approach. The average arc of forearm rotation was 142.30 in our study compared to 129.60 by Muhammad Haseeb et al5 and 1500 by Goldfarb et al.9 The average arc of wrist motion is 142.80 in our study compared to 140.10 by Muhammad Haseeb et al 5 study. All but one radius fracture were unitted at the end of six months which is also unitted at 9 months without any intervention. No vascular or nerve injury in our study group. No superficial or deep infectionin our analysis. Hadden et al 8 reported nonunion in 3%, infection in 5.4%, and nerve injury in 6.3% in his study which included 111 patients. Chapman et al 6 reported nonunion in 2% and infection in 2.3% in his study.
Functional and radiological outcome of our study results are comparable to the studies using the standard volar and dorsal approaches. Complication rates in ourstudy are lesser as compared to other studies. Lateral approach is comparatively easier as the surgical plane is devoid of vital neurovascular structure. The modified lateral approach described by Backiaraj Devaraj et al10 eliminates the theoretical risk of injury to superficial radial nerve by lateral approach.4 Modified lateral approach with lateral plating of the radius is a viable alternative to the conventional techniques. But further long term prospective comparative studies with larger patient numbers are needed to confirm our results.