Introduction
Total hip arthroplasty represents about 1.5 million surgeries performed worldwide each year. It is one of the most successful procedure, some concerns remain though. The two main total hip replacement related issues are dislocation and wear.
Dislocation may be described as the extraction of the replaced femoral head from the acetabular cup. The ligament in charge of preventing this phenomenon in the native hip is no longer present in the operated hip.
To address this particular problem of dislocation, Pr. Gilles Bousquet and André Rambert shared their knowledge to invent the dual mobility concept patented in 1975.1 This innovation has enabled to improve the range of motion and to significantly reduce the number of dislocations even though this postoperative complication depends on several factors other than design-related ones. Thus this solution seems to be promising for reducing the risk of instability.
However, intraprosthetic dislocation* has appeared as a new issue and wear still remains a concern. Indeed wear is known to entail osteolysis because of the particles release. Therefore the concept of dual mobility has to be kept improving.
Currently dual mobility cup are well accepted treatment options for patients at higher risk of dislocation, neuromuscular diseases, cognitive dysfunction, all patients older than 75 years with a history of prior hip surgery, in revision THA for any cause, primary THA after femoral neck fracture, and primary THA after tumour resection.2
The purpose of this study is to demonstrate the performance and reliability of “DUAL MOBILITY CUP” used during Total hip arthroplasty.
Materials and Methods
It is a hospital based prospective study of 20 patients diagnosed clinically and radiologically with conditions require THR between Nov 2017 – Jan 2020. All the patient who received a dual mobility cup between Oct 2017 and Oct 2019 in hospitals attached to Bangalore Medical College & Research Institute, Bangalore were studied for a duration of 12 months. The functional outcome was assessed with HARRIS HIP SCORE and PMA SCORE. The data was analyzed using descriptive statistics.
Inclusion criteria
Patients of age 18 years and above of either sex.
Patients diagnosed clinically and radiologically with below condition:
Primary and secondary osteoarthritis of hip.
Failed fixation of proximal femur fracture.
Femur head necrosis.
Femur neck fracture in elderly who are not ideal for osteosynthesis.
Rheumatoid arthritis of hip.
Ankylosing spondylitis of hip.
Willingness and written informed consent of the patient to participate in the study.
Methodology
Patients who fulfils the inclusion criteria will be taken into the study after obtaining written informed consent. Demographic data, history, clinical examination and details of investigation and intervention will be recorded in the study performa.
Patients were followed on 6 weeks, 3 months, 6 months, 1 year.
Statistical method
Data collected was tabulated and Categorical variables were expressed in terms of percentage and proportion. Continuous variables are expressed in terms of mean and standard deviation and data was analysed using descriptive statistics.
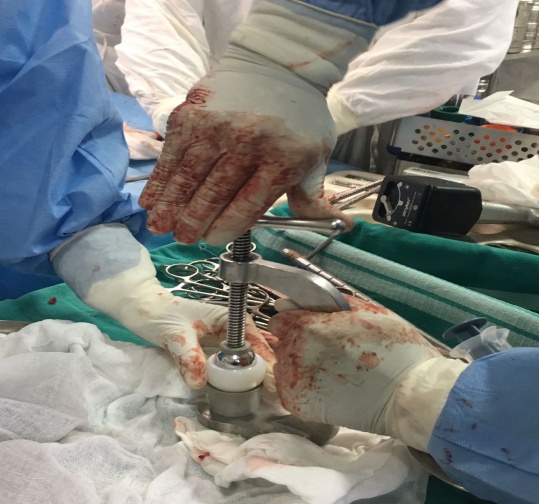
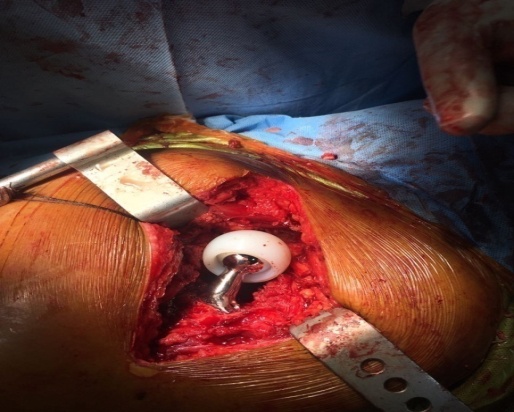
Surgical procedure
All surgeries were performed on an elective basis using standard aseptic precautions and surgeries were either performed under spinal with epidural or general anaesthesia.
Lateral position with the patient laying on the unaffected side. The skin over the hip was scrubbed with povidone-iodine.
Approach: Moore’s Approach (Southern Exposure)
Postoperative management
Pharmacologic prophylaxis for prevention of DVT (ACCP guidelines) Intramuscular analgesics were given as per patient's compliance; intravenous antibiotics were given (2 doses – start with preop and postop 1 dose).
Check radiograph was taken after 48 hours. Dynamic quadriceps exercise, standup with support (walker), on the first or second day, and were allowed to full weight bear and walk with the help of a walker depending on his/her pain tolerance and were encouraged to walk thereafter. Sitting cross-legged and squatting were not allowed.
Patients were followed up at an interval of 1 month, 3 months, 6 months, and 9 months and functional outcome was analyzed by modified Harris hip scoring system and PME scoring system. At each follow up radiograph of the hip was taken for radiological analysis.
Observations and Results
The following observations were made from the data collected:
Age incidence
Maximum age was 82 years and minimum being 53 years, with mean age of 63.28 years in male an 65.56 years in females.
Mean age: 64.30 years and standard deviation 7.4 years.
Sex incidence
In our series there were 9 female patients and 11 male patients.
This show preponderance of Males over Female patients.
Type of implant fixation technique used
Table 4
Fixation technique used distribution of patients studied
| Implant | No. of patients | % |
| Cemented | 8 | 40.0 |
| Hybrid | 4 | 20.0 |
| Un cemented | 8 | 40.0 |
| Total | 20 | 100.0 |
Table 5
HHS
Table 6
PME score
Functional outcome
In our study the HHS improved from mean value of 63.89 in first month to mean value 90.3 as in 12 months and 11 patients shows excellent outcome at the 12th month follow up with p value < 0.001.
In our study the PME score improved from mean 12.26 in first month to mean value of 15.72 as excellent in 12 months. 1 patient show poor outcome at 1st month follow up and18 patients show Excellent outcome at the end of 12th month
Discussion
Total hip arthroplasty represents about 1.5 million surgeries performed worldwide each year. It is one of the most successful procedure, some concerns remain though. The hip joint and the surrounding can be affected by a disease or a fracture that requires the replacement of this particular ball-and-socket joint, which is done using a total hip replacement (THR). This procedure is one of the most common and successful as it is demonstrated by the increasing number of such surgeries world-wild each year. Several types of THR are currently used, they vary in the materials, the geometries, the number of mobility and so on.
To this purpose, we evaluated the functional outcome in addition to surgical outcomes in patients treated with total hip arthroplasty by using dual mobility components. The results were analysed and observations were made.
Out of the twenty patients one patient was lost to the follow up and one patient died 2 days postoperatively with acute renal failure. This study was compared to similar studies by other authors.
The functional outcome in the study was measured by Harris Hip Score and PME score which uses a set of daily activities to gauge the level of function after surgery.
Table 9
In this study the HHS showed a consistent improvement from
In this study the PME score showed a consistent improvement from
At the end of the study 100% patients shows Excellent PME score outcome.
In a study done on Unconstrained tripolar Implant’s for primary total hip arthroplasty in patients at risk for dislocation consists of 167 primary total hip arthroplasty shows the mean preoperative HHS improved from 39.6 to 83.4 at the least follow up.
In a study by R. A Rasheed et al.3 -included 31 patients (32 hips) with displaced femoral neck fractures that were admitted to El Hadara University Hospital, Alexandria, Egypt The mean HHS improved over the follow up period from 79.04 +/- 7.9 at 12 weeks to an average of 92.8+/- 11.1 at 1year follow up. They concluded that Dual mobility cup total hip replacement is an acceptable method for treatment of displaced femoral neck fracture in active middle aged patients in Egypt as it provides pain relief and good function without compromising the stability.
In a study done by G Canton, A Moghnie, M. Cleva, et al4 on Dual mobility total hip arthroplasty in the treatment of femoral neck fractures shows Harris Hip score showed a mean value of 81,22 (range 54,60-97,02). They concluded that good clinical results, low complications and very low dislocation rate with Dual mobility total hip arthroplasty for neck of femur # treatment at longer follow- up.
In our study HHS and PME score have similar values in patients <60 years of age and >60 years of age (P >0.005) and at the end of 12th month HHS and PME score for different diagnosis have similar score (P>0.005).
In a study done by Sarunas Tarasevicius et al.5 Of the 620 dual-mobility with Median follow-up time was 2.5 (0–5) years concluded that THA DMCs are reported to have a high rate of loosening and a higher rate of osteolysis and cup loosening in younger patients and cases of childhood disease sequelae.
They also found that surgery for diagnosis other than OA had an increased risk of revision, suggesting that dual articular cups could be considered for non-OA patient, e.g. for THA due to femoral neck fractures.
In our study Cemented, Cement-less, Hybrid, technique of implantation shows similar HHS score and PME scores at the end of 12th month (P>0.005) and PME score of both male and female at the end of final follow up have similar HHS (P >0.005).
In a study conducted by Divyanshu Goyal et al.6 in a hospital based, randomised, comparative type of observational study, on functional outcome of cemented and un cemented total hip replacement in which 25 patients were included in each group for a follow up duration of 2 years, they concluded that better short-term clinical outcomes mainly improved pain and early pain-free full weight bearing was obtained from cemented fixation.
In our study one patient sustained peri-prosthetic fracture (Vancouver AL) one during broaching of proximal femoral medullary cavity in dual mobility THR with press fit uncemented stem and the same was augmented with SS wire, One patient developed surgical site infection at operative site, same has been treated with regular dressing and antibiotics according to culture report.
One patient died postoperatively and one patient shows radiologically new bone formation at femoral side and lysis around the acetabular component. Rest of 17(85%) patients had no complications related to total hip arthroplasty.
A systematic review of comparative studies of dual-mobility constructs in primary and revision total Hip arthroplasty for primary THAs, the overall rate of dislocation was 0.9% in the dual-mobility group compared to 6.8% in the control group (p<0.001) at a mean follow-up of 7.6 years. The odds ratios for the control group to the dual-mobility group were 4.06 (p<0.001) for dislocation, 1.18 (p=0.87) for revision, 2.97 (p=0.04) for revision due to dislocation, 1.67 (p=0.57) for infection, 0.6 (p=0.53) for fracture, and 1.21 (p=0.81) for aseptic loosening.
In our study Implant survivorship is 94.9% at the end of final follow up. In a study conducted by Chahine Assi 7 et al. on Outcomes of dual mobility cups in a young Middle eastern population and its influence on life style, the survival rate of DMC implants is found to be 100% in a follow up of 60 months.
In a study by B. Darrith et al.8 on a systemic review of Outcomes of dual mobility components in total hip arthroplasty, for 10783 primary dual mobility THAs the overall survivorship of the acetabular and dual mobility components was 98.0% at a mean follow-up of 8.5 years.
Conclusion
Dual mobility cup total hip replacement is an acceptable method for patients who are planned for Total Hip Arthroplasty as it provides pain relief and good function without compromising the stability.
Use of dual mobility cup in total hip arthroplasty is increasing shown good results in the short term follow up (Good to Excellent) compared to conventional total hip replacement.
High-quality, prospective, comparative studies are needed to evaluate further the use of dual mobility components in THA.