Introduction
In patients with total knee arthroplasty(TKA), any mass occurring in and around the knee joint needs thorough assessment. The differential diagnosis include hematoma, infection, Morant-Baker's cyst, ganglion cyst, semimembranosus bursitis, popliteal artery aneurysm, primary soft tissue or bone tumors, thrombophlebitis, cellulitis and deep vein thrombosis. In post knee arthroplasty scenario, pseudotumor mass or a wear debris induced cyst, should also be considered. Characteristic findings on physical examination as well as radiologic and serologic examinations can make the diagnosis straightforward in most of the cases. We report a case of failed TKA that presented as a cystic swelling in the calf region without much knee symptoms, three years after primary TKA.
Case Report
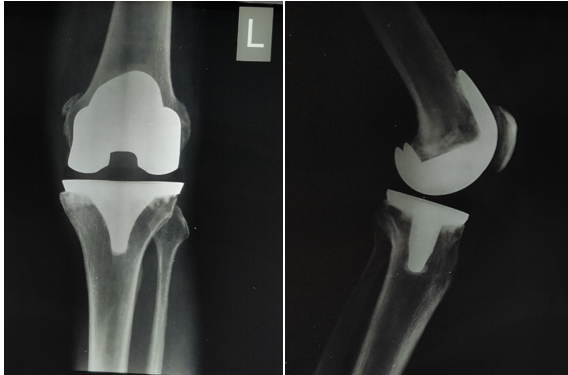
A 75 year old male patient presented to us with complaints of a progressively enlarging swelling in his left calf region of three months duration. He had undergone left total knee arthroplasty (posterior stabilized, Exactech Optetrak prosthesis, Florida, USA) for tricompartmental osteoarthritis three years back (Figure 1). Three months ago, the patient noticed a small mass developing around his popliteal fossa with intermittent swelling of the knee joint. There was a progressive increase in size of the swelling. He experienced restriction in knee movements in the last one month following which he presented to us for evaluation. There were no constitutional symptoms.
On examination, there was a 20cm x 10 cm soft tissue swelling extending from popliteal fossa to the mid calf region of the left leg (Figure 2). The swelling was cystic with a smooth surface, non tender and non-pulsatile. Mild effusion was noted in the left knee joint without any signs of inflammation. Active knee range of motion was limited to 50 - 900, with normal distal neurovascular status. Radiographs showed loss of joint space mainly on the medial side between the femoral and tibial components, periprosthetic osteolysis of the distal femur and a large soft tissue shadow in the popliteal and calf area (Figure 3). A doppler ultrasound scan ruled out deep vein thrombosis. An MRI scan revealed a large cystic mass of size 18cm x 9cm x 7cm expanding from the gastrocnemius-semimembranosus bursa and extending into the calf between the gastrocnemius and soleus muscles (Figure 4). Blood investigation showed a normal white blood cell count (TC=5000/ mm3), normal erythrocyte sedimentation rate(ESR= 5mm/hr) and C-reactive protein(CRP= 0.3mg/L) levels. The coagulation parameters were within normal limits. With the presumptive diagnosis of polyethylene lysis and aseptic loosening of femoral component associated with a calf mass, the plan was to proceed with a two stage procedure- 1) excision of swelling with microbiologic and histopathologic examination, followed by 2) definitive procedure after getting the lab reports.
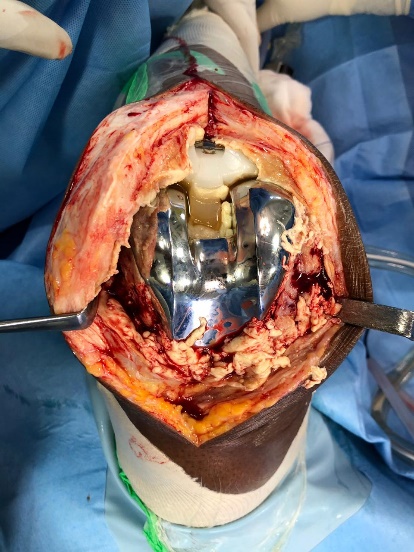
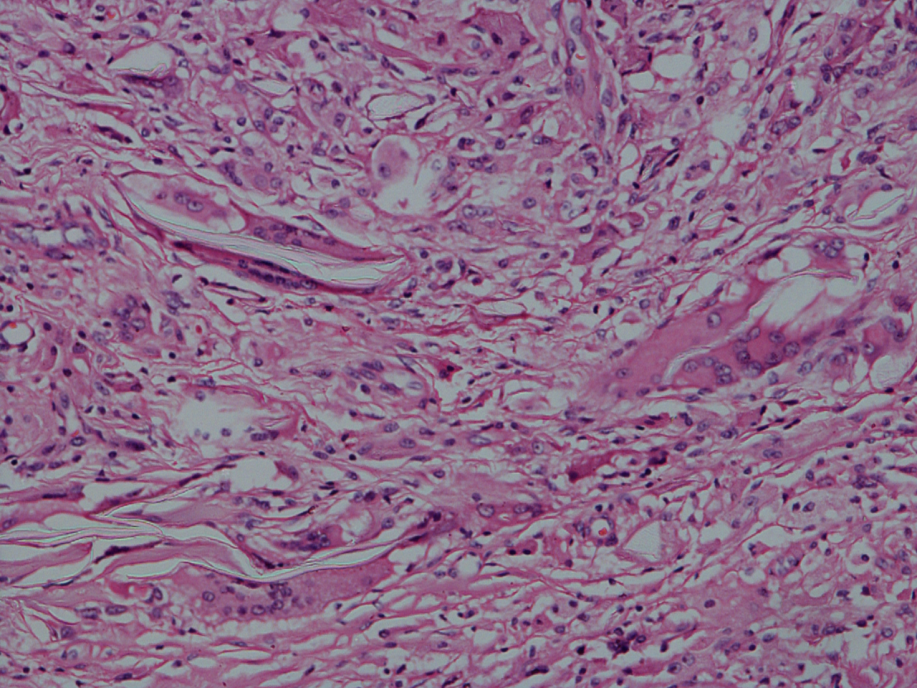
The cystic mass was approached through a posteromedial approach. Per-operatively, the cystic mass was communicating with the posteromedial knee joint (Figure 5). The mass was excised and it contained around 1000ml thick yellow fluid with polyethylene debris and necrotic material (Figure 6). Microbiological evaluation was negative and histopathologic examination showed multinucleated foreign body giant cells around refractile material without atypia, consistent with the picture of a tissue response to artificial joint implants (Figure 7).
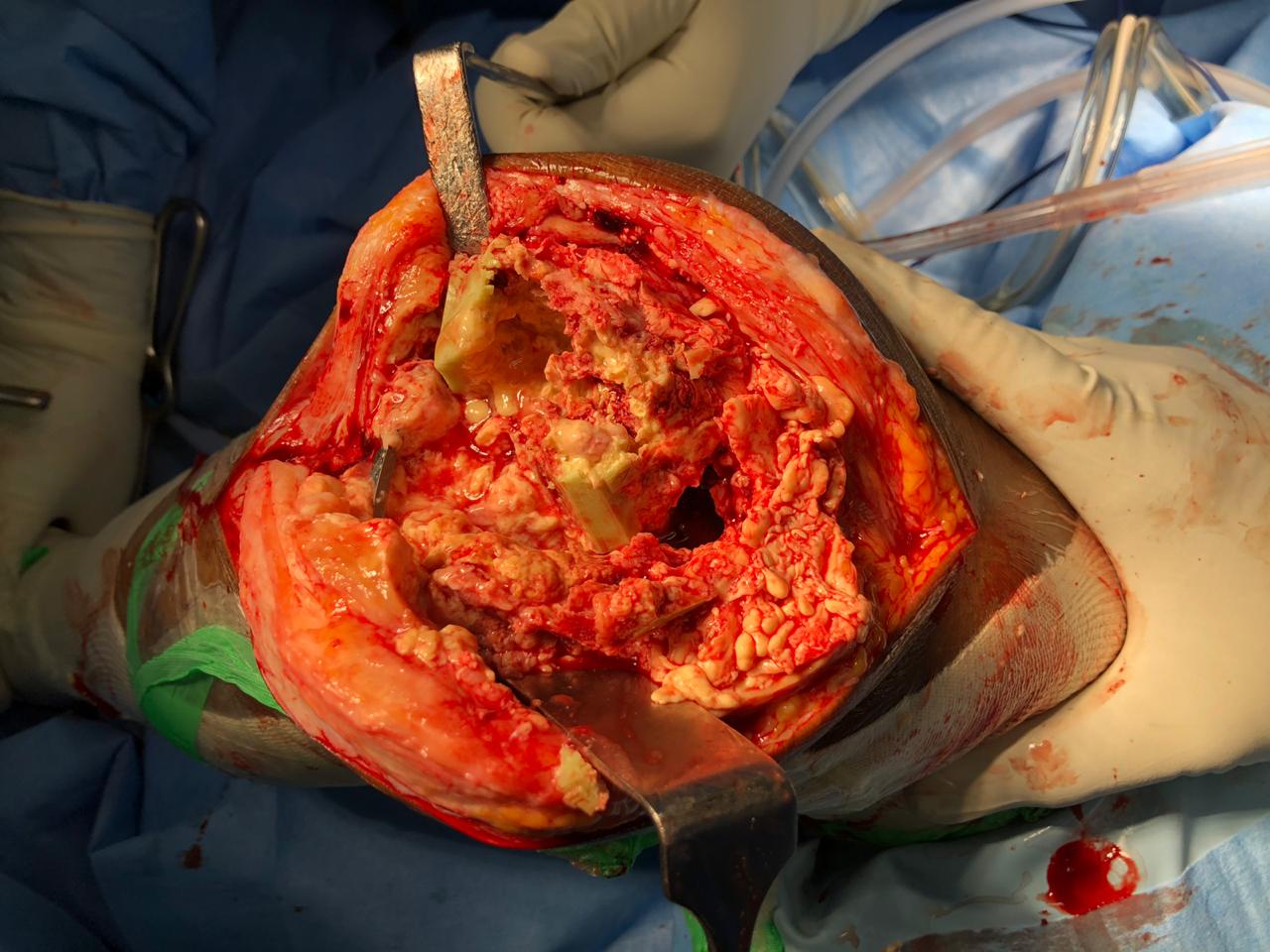
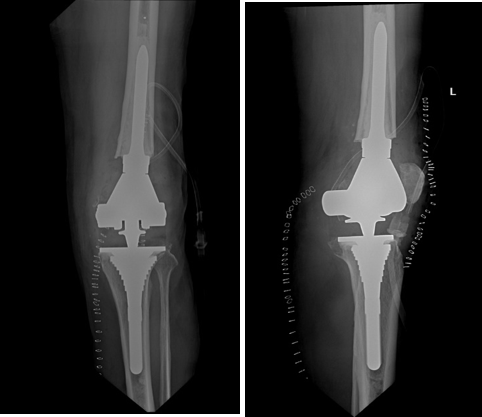
After having an uneventful soft tissue healing, revision knee arthroplasty was performed through a medial parapatellar approach. Peroperatively there was extensive synovial hypertrophy without any metallosis (Figure 8). The polyethylene insert had gross pitting and delamination along with tibial post wear and backside wear (Figure 9). After extensive synovectomy, loosenened femoral and tibial components were carefully removed. Extensive bone loss along with loss of integrity of medial collateral ligament was noted on the femoral side (Figure 10), for which a Distal femoral replacement component (LPS, Depuy Orthopedics, Warsaw, USA) was used and the tibial side bone defect needed a metaphyseal sleeve and stem with a MBT revision tray (Figure 11). There was uneventful postoperative recovery. At one year follow-up, there was pain free joint movements with range of 00–1100. There were no signs of cyst recurrence.
Figure 3
Pre- operative radiographs show loss of joint space between femoral andtibial components, periprosthetic osteolysis on both distal femur and proximal tibia, along with a soft tissue mass shadow in the posteromedial aspect

Figure 4
MRI images of the left leg showing large cystic mass extending from popliteal fossa to midcalf, communicating with the knee joint
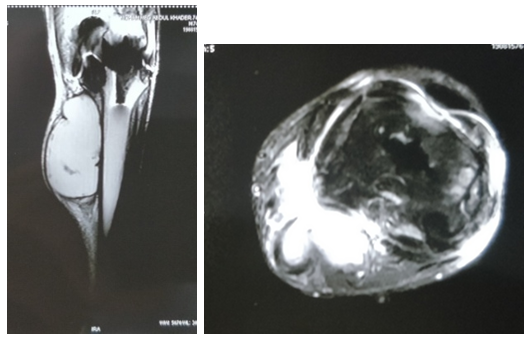
Figure 5
Intraoperative photograph after excision of thecystic mass showing plane between the medial gastrocnemius and semimembranosus

Figure 6
Image showing (a): Cystic mass (18cmx9cmx7cm) excised from the leg, and (b): Turbid fluid containing coarse granules evacuated from the cystic mass
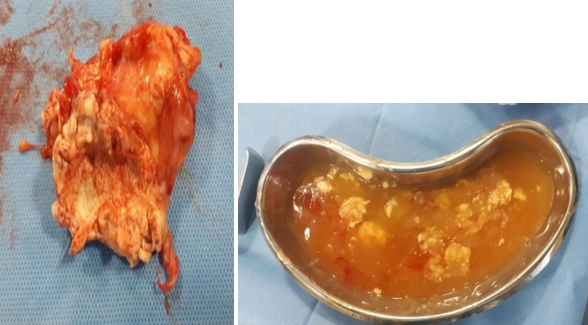
Figure 7
Histo-pathologic section shows a foreign body reaction with giant cells around refractile material
Discussion
A leading cause of total knee arthroplasty(TKA) failure is attributed to aseptic loosening from polyethylene wear disease. Mechanical wear patterns of the implanted high-molecular weight polyethylene(UHMWPE) include pitting, scratching, burnishing, abrasion and delamination, which can all liberate numerous fine polyethylene particles. This wear debris induces macrophage phagocytosis that triggers an inflammatory reaction within the knee joint which can lead to synovitis, repeat effusions and ultimately, to aseptic loosening.
In this setting, pain and swelling of the knee joint are usually the most common presenting symptoms. However, atypical manifestations such as a popliteal cyst, bursitis, calf mass, or thigh mass can be the presenting symptom, making the initial diagnosis difficult. Dissecting popliteal cyst associated with failed TKA was reported by Dirschl et al,1 Moretti et al,2 Niki et al,3 Chan et al4and Tofte et al.5 Failed TKA presenting with calf mass was reported by Akisue et al,6 Chang et al7 and Choi et al.8 Bursitis and thigh mass due to polyethylene wear disease were reported by Huang et al9 and Chavda et al10 respectively. These masses have been reported two to eight years following the primary joint replacement. In all cases, as in our case, the final diagnosis was foreign body reaction due to polyethylene or metal wear debris.
The high intraarticular pressure caused by particle-induced joint effusion contributes to a popliteal cyst formation. Pseudotumor like mass may be formed due to a granulomatous inflammatory reaction to excessive wear particles generated. Fluid pressure arising from the joint allows the particles to track along soft tissue planes giving rise to a gradually enlarging mass someway distant from the joint. These masses may attain large size causing pressure symptoms. In the present case, synovial fluid with polyethylene wear particles from the joint, drained underneath the fascia and the medial head of the gastrocnemius muscle in the popliteal fossa and progressively enlarged into the calf region with increased wear particle generation.
The factors that influence implant wear include: patient factors (age, activity and weight), implant factors (type of articulation, design, bearing surfaces, polyethylene thickness and method of sterilization), and surgical factors (alignment and ligament balancing). Any combination of these factors may result in the generation of significant quantities of particulate debris. In the reports reviewed, the causes for wear generation were- young age, high activity level,6, 8 thin polyethylene insert(<8mm), polyethylene oxidation6 and malaligned tibial tray. In our case, lack of regular follow-up led to the delay in the diagnosis, ultimately contributing to the formation of a huge mass and extensive osteolysis. The paucity of subjective symptoms such as pain and minimal knee effusion obscured the clinical picture.
In terms of treatment for failed TKA with the symptom of an extraarticular mass, single stage or a two-stage revision was recommended by different authors with good results. Niki et al3 advocated synovectomy and polyethylene liner exchange in a patient with implant well positioned and well fixed. Dirschl et al1 reported about three patients who underwent a revision of TKA without excision of the popliteal cyst. Chan et al4 was the first to advocate a two-stage procedure for the treatment of a large dissecting popliteal cyst after failed TKA, cyst excision in the first stage followed by revision TKA after few weeks. The rationale behind this management was to first relieve the pain caused by large cyst, and also eliminate the polyethylene debris-induced factor causing osteolysis and prosthesis loosening. Moretti et al2 also recommended a two stage procedure with a long-term interval of five months between the stages in case of very old patients, particularly those with medical co-morbidities. We followed the recommendation of Chan et al and performed a two-stage procedure to make sure that there is no active infection at the time of revision implantation and also to allow for better wound care in this elderly patient.
Conclusion
This case report illustrates how polyethylene wear disease after TKA can manifest as a rapidly enlarging, massive cystic swelling in the posterior compartment of the leg. Our patient underwent a two stage surgery, excision of cyst followed by revision implantation which resulted in a good functional outcome.
Wear debris induced cyst or a pseudotumor mass must be included in the differential diagnosis of a swelling around the knee joint in post knee arthroplasty scenario.
Regular follow-up examination after TKA, with careful clinical and radiological assessment is critical for early detection of occult polyethylene wear and prosthesis loosening.
Joint effusion and the subsequent synovial cyst formation should be considered a preceding sign of periprosthetic osteolysis, component wear, as well as prosthetic loosening.