Introduction
Lateral epicondylitis(LE) is a condition in which patient has pain in the lateral aspect of the elbow, more precisely over the common origin of the extensor muscles of the wrist and fingers.1 The condition affects both sex equally. It is associated with the chronic overuse of the extensors of the forearm, however factors such as microvascular trauma, cutaneous nerve injury and friction wear of the extensor carpi radialis brevis muscle (ECRB) have been proposed. 2
Currently, numerous methods are suggested in the treatment of LE from local injection to various surgical techniques. 2, 3 However, very few methods have been scientifically proven to be effective and there is a lack of evidence proving one technique’s superiority over another. Lateral epicondylitis has displayed slight response to physiotherapy, hot fomentation, and analgesics in some patients. However, frequently this condition is resilient to treatment which causes a prolonged period of functional restraint. The various methods of management of LE includes local injections with Platelet rich plasma, autologous blood, corticosteroids, short wave diathermy, ultrasound therapy and local anesthetic agents.4 Local steroid injection has been shown to give a consistent, predictable short-term relief from the pain, and the movement limitation.5
In the current study, we compared the effectiveness of peppering technique with single injection technique by using steroid along with local anaesthetic injection in the treatment of chronic lateral epicondilitis(LE) of Elbow.
Materials and Methods
This prospective study was conducted among 66 patients who were diagnosed as chronic tennis elbow in the age group 20-70 years of either sex attending orthopedic outpatient department at Sree Mookambika Institute of Medical Sciences. Patients were diagnosed based on positive history and relevant clinical examination. All patients provided informed consent in the language he or she understands.
Patients with significant pain and tenderness over the common extensor origin in the elbow, a positive chair test,6 a positive Mills’ sign7 and positive Cozen’s test8 and cases with tennis elbow in the chronic stage, i.e. duration of pain more than 6 months and failed to respond to NSAIDS drug therapy and physical therapy were included in the study.
Patients with arthritis, calcifications or any fracture or bony abnormality or any effusion or infection of the elbow joint, patients with bleeding disorders, carpal tunnel syndrome, radial tunnel syndrome, uncontrolled Diabetes Mellitus, patients who has taken previous injection and surgery for lateral epicondylitis and those on anticoagulant therapy and cervical radiculopathy were excluded from the study. Magnetic resonance imaging study was not included in the study.
The first 33 patients (SNI group) were treated with local injection of 1ml of methylprednisolone acetate 40 mg (Steroid) and 1 ml of 2% lignocaine(local anesthetic) at the maximal point tenderness at lateral epicondyle by single-injection technique and the next 33 patients (PRI group) were treated with local injection of 1ml of methylprednisolone acetate 40mg (Steroid) and 1 ml of 2% lignocaine(local anesthetic) at the area of maximum tenderness at lateral epicondyle by peppering injection technique. All the patients were blinded by type of injection.
The patients were instructed about the treatment side effects and possible complications and also the study procedures in patient own language. Patients’ demographic and occupational data were collected and patients were evaluated with initial assessment of Visual analogue scale (VAS). After the procedure all patients were instructed to rest the elbow and wrist for 48 Hrs. No additional medications were given for the patients. All the patients were followed up and reviewed at the end of 2nd week, 6th week and 6th month after the initial therapy and were assessed by routine clinical history and marked level of pain from 0–10 on the visual analogue scale (VAS) of pain, where zero indicates complete absence of pain and ten the worst pain. [Figure 1]
The outcome was compared with the pre-injection condition. The improvement in pain was graded based on the amount of change in VAS score. We considered lack of improvement if the VAS score remained same from the baseline or showed an increase in the severity. [Table 1]
Table 1
Grading of VAS Score
|
VAS score change |
Outcome |
|
More than or equal to 3 |
Good |
|
More than or equal to 2 |
Moderate |
|
More than or equal to 1 |
Mild |
Injection technique: Peppering injection technique is done with patient in supine on an examination table with affected elbow in 90° flexion and hand in neutral rotation. Under sterile aseptic precautions, 1 ml of Inj. Methyl prednisolone acetate I.P. 40mg with 1ml of 2% lignocaine is peppered using an 18-gauge needle, which is introduced exactly at the point of maximum tenderness.[Figure 2] The needle is inserted, injected and then slightly withdrawn without coming out of skin and then needle direction is changed and again injected, this is repeated multiple times(40-50 shots) until crepitus or crackling felt initially was lost.[Figure 3] The needle should be handled gently to avoid damage to tip of the needle, if the bone is contacted. 9
The mechanism of action of peppering injection technique is attributed to local bleeding and hematoma formation by multiple injections (peppering) through the granulation tissue and degenerative tendons. This bleeding starts healing process of the area of tendinosis.10, 11 The mechanical disruption caused by peppering injection may transform a failed intrinsic healing process into an extrinsic response. 12, 9
Statistical analysis: The Statistical Package for the Social Sciences (SPSS) version 24 software was used for all statistical calculations. Repeated measures ANOVA was used to check the difference between the two different techniques and to compare the VAS score changes before and after injection within the groups. Profile plot, descriptive statistics and graphs are given. A p-value < 0.01 was considered statistically significant.
Results
The study group of 66 patients had 32 male and 34 females. [Figure 4] Most of the patients were in the age group of 30-50 years with mean age of 43.3 ± 9.3 years. [Figure 5] Patients had complaints of pain for a mean duration of 9.4 ± 2.9 months. The right elbow was affected in 46 patients whereas 20 patients had left elbow pain and no one among the study population suffered bilateral disease.
The mean VAS score of SNI Group on pre injection was 4.30 (± 0.081 SE). The mean VAS score observed at 2 week, 6 week and 6 months follow up was 3.66 (± 0.06 SE), 1.63 (± 0.131 SE) and 1.42 (± 0.118 SE) respectively. After application of Repeated Measure ANOVA Test, the p value for the reduction in mean VAS score came out to be less than 0.01 suggesting a statiaticlly significant decrease in pain level at 2 weeks, 6 weeks and 6 months follow up as compared to the initial pre-treatment score in SNI Group.[Table 2]
Table 2
VAS Score of SNI group
In PRI Group the pre injection mean VAS score was 4.69 (± 0.081 SE). The mean VAS score observed at 2 week, 6 week and 6 months follow up came out to be 3.90 (± 0.06 SE), 1.90 (± 0.131 SE) and 1.12 (± 0.118 SE) respectively. After application of Repeated Measure ANOVA Test, the p value for the reduction in mean VAS score came out to be less than 0.01 suggesting a significant decrease in pain level at 2 weeks, 6 weeks and 6 months follow up as compared to the initial pre-treatment score in PRI Group. [Table 3]
Table 3
VAS Score of PRI group
At the 6-month follow-up mean VAS score measured were 1.42 in group SNI as compared to 4.30 before the commencement of the treatment and 1.12 in group PRI compared to pre-treatment scores of 4.69. The difference between the groups in VAS score at the end of six months was statistically significant (P < 0.001). [Figure 6]
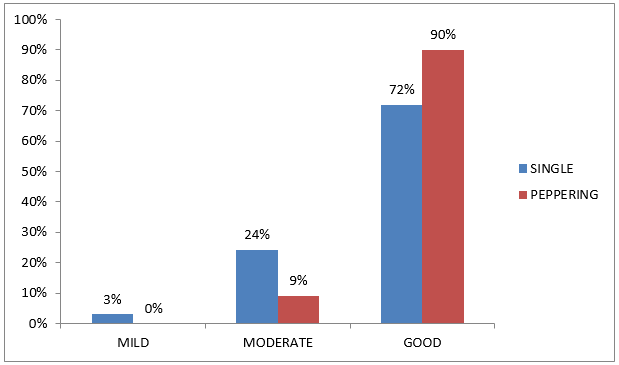
The rate of good result was higher in PRI group than SNI group. [Figure 7] All patients found the injection painful. In our study 12 patients(SNI group) had skin dis-coloration and 7 patients reported transient itching at the site of injection, whereas these complications does not alter the VAS score outcome.
Discussion
The main finding in our study was that peppering technique (PRI group) was effective than single injection technique (SNI group) in the treatment of chronic lateral epicondylitis, with injection of local anaesthetic and steroid combined, for those patients who were not responding to any of the various conservative therapy. Local steroid injections have been used in the management of patients with lateral epicondilitis, with varying results. Verhaar et al., 13 in a prospective, randomized trial on 106 patients compared the effect of combined local anesthetic with local steroid injection with physiotherapy and concluded that the injections were more effective than physiotherapy. Smidt N et al., 14 in their randomised controlled trial “Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial” found that the corticosteroid injection gave better results than physiotherapy and wait and see in treatment of lateral epicondylitis in short term.
Tonks JH et al., 15 in their prospective randomised controlled trial “Steroid injection therapy is the best conservative treatment for lateral epicondylitis: a prospective randomised controlled trial” found Patients those who were treated with steroid injection had better outcome at follow up, in addition there was no influence of physiotherapy nor benefit of combining physiotherapy and injection was recognized, therefore they recommend steroid injection alone as the first line of treatment for patients presenting with lateral epicondylitis. Also Olaussen, M et al., 16 in his randomised controlled trial, “Corticosteroid or placebo injection combined with deep transverse friction massage, Mills manipulation, stretching and eccentric exercise for acute lateral epicondylitis: a randomised, controlled trial” concluded that in those patients who demands a quick improvement, corticosteroid injections along with the physiotherapy treatment can be considered.
In our study, at 2-weeks and 6 weeks follow-ups, the intra group statistical analysis showed a significant reduction in mean pain VAS score in both SNI and PRI groups when compared to the pre-injection score. This shows the efficiency of corticosteroid injection with local anaesthetic agent in the management of chronic lateral epicondylitis in short duration as evident by many studies. 15, 16, 17, 18 This outcome of corticosteroid injection with local anaesthetic is enhanced by giving the injection using peppering technique for 6 months. This is supported by the prospective randomized study of Altay et al., 9 “Local injection treatment for lateral epicondylitis”, in which they found that at the end of 6 months follow-up, patients received peppering technique injection of local anaesthetic alone had 93% excellent result whereas it was 95% in patients who received corticosteroid in addition to local anaesthetic by peppering technique and this excellent outcome in both the groups shows the effectiveness of peppering technique. Moreover, they suggested that the peppering technique of injection is effective technique for conservative management of lateral epicondylitis of elbow. 9
At 6-month follow-up in this current study, the good results were 90%(n=30) in the peppering injection technique group (PRI group) and 72% (n=24) in the group treated with single technique injection (SNI group)(Graph IV). Thus, the success rate for Peppering technique is significantly higher than the single injection technique of local anaesthetic with corticosteroid. This is similar to the findings of Dogramaci et al., 19 who in his randomized prospective clinical trial “Treatment of lateral epicondlitis using three different local injection modalities: a randomized prospective clinical trial” reported a significantly lower pain (VAS) at 6 month follow-up in patients treated by combination of local anaesthetic and corticosteroid injections with peppering technique than all other groups i.e. single local steroid injection and local anaesthetic alone by peppering technique. Similarly Okçu G et al., 20 in his a prospective randomized clinical trial “Evaluation of injection techniques in the treatment of lateral epicondylitis: a prospective randomized clinical trial” showed that clinically successful outcome depends on the injection method, rather than the corticosteroids and also peppering technique is more effective than the single injection technique, in the long-term. Multiple injections reach the bone through the degenerative tendons and granulation tissue, causing local bleeding. It is believed that this bleeding organize to form a hematoma, which may initiate a healing process.
The results of our study shows that, the local corticosteroid injection turn out to be more effective when given by peppering technique, in treating the patients with chronic lateral epicondylitis than single injection technique, in follow up of 6 months.
Conclusion
In our study we conclude that peppering injection technique is better than single injection technique in terms of reduced pain which was assessed by VAS in the treatment of chronic lateral epicondylitis of elbow in the long-term follow up. When local corticosteroid injection is considered as option in the management of lateral epicondylitis elbow, peppering technique is the effective choice, as it has the highest good result in long term, than single injection technique.