Introduction
In an era of advanced orthopaedic care, native bone setters are still one of the largest group practicing traditional medicine in many developing countries. 1, 2, 3 Even in a country like ours with abundant of medical institutes and with the best advance medical care, about 60% of traumas are treated by native bone setters. 2
There are many native bonesetters practising centres present and still more getting open all over India. 3, 4 Mostly about 10-40% of patients around the world prefer ancient ways of healing fractures. 1, 2, 3 Native bone setters are people who uses ancient method of healing bone fractures and have been existing over more than 3000 years and still famous among the rural people. 1, 2, 3 Native bone setters in Ghana are considered to be as, an important individuals in treating fracture among thousands of people before the existence of modern health care services. 5 In Nigeria, native bone setters attended to rural patients in about 90% of primary healthcare centres. 6 Native bone setters are preferred for fracture treatment by the people of Bangladesh as they give importance to traditional belief. 7 It is believed that native bonesetter practices a special type of ancient medicine. 7, 8, 9 Native bone setters still gains popularity in most of developing countries because of low cost, easy accessible, cultural believes and strong influence from families and friends. 4, 5, 6, 7, 8, 9
Native bone setters are practitioner who manipulates fractures and dislocation. 3, 4 The native bone setters are unqualified, inherited the method from their ancestor for generations and others join as apprentice and learn the trade on hand. There were no proper documentation of their procedures. 6, 7, 8 Most of these native bone setters had no idea about the human anatomy, physiology, prevention or control of infection which is the main reason for increase failure rates and complications. 8, 9
The principle method of management used by the native bone setters for immobilization is to applying a tight splint to the fracture site, the materials they use includes like bamboo, rattan cane or wooden pieces, along with cotton pieces dipped in different types of herbal oils, these materials are put together to form a roll like splint and wrapped around with palm leaf axis sticks consequenting tourniquet effect. 6, 7, 8, 9, 10, 11 Other methods like massaging with herbal oil and some weird methods the use of incantations and scarification. 10, 11
Complications due to native bone setter’s management may arise during or after treatment as a result of improper diagnosis, improper stabilizing, improper technique and with no proper rehabilitation.12, 13 These complications may be acute and chronic like Compartment Syndrome, Tetanus, Deformities, Chronic Osteomyelitis, Gangrene, amputation and some may even lead to death.14, 15, 16, 17, 18, 19, 20, 21 This study was conducted to evaluate why patients prefer native bone setters treatment and to identify common complications associated with it.
Materials and Methods
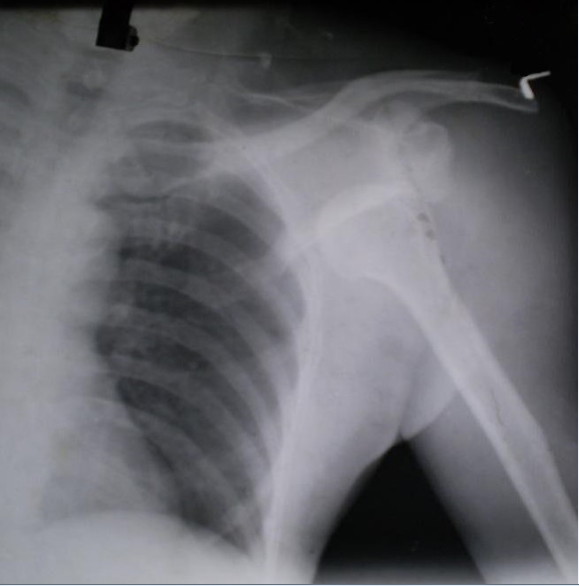
A Retrospective study done on datas of 362 patients who were admitted after having initial treatment done from native bone setter in the orthopaedic department in a tertiary medical care hospital from September 2016 to September 2019 Patients were selected based on inclusion criteria. The inclusion criteria were Patients should present with upper or lower limb fractures or dislocations with initial treatment done by native bone setter. Documentation of clinically examined and evaluated of the site of fracture or dislocation notes should be present, xray of the site of fracture or dislocation be present. Observational notes should be documented regarding complications like infection, compartment syndrome, fat embolism syndrome, gangrene, pressure ulcer, malunion, delayed union, nonunion, joint stiffness, osteomyelitis and neuropathy. All patients should have routine blood investigation performed. Written documentation of acquired consent for the surgery, post operatively management and discharge summary, follow ups and the outcome after the management should be noted. The exclusion criteria included pregnant women, fracture or dislocation associated with head injury/chest injury/abdominal injury/spinal injury, Loss of important documented data mention in the inclusion criteria.
Results
The Retrospective study done on 362 patients who came to the emergency casualty or attended orthopaedic OPD. These patients had presented after 10 -14 days after taking treatment from native bone setters because they were not satisfied by their treatment due to persistent pain and difficulty in their movement. In 362 patients, 221were males (61.04%) and 141were females (38.95%). The male to female ratio (1.56:1). Their ages ranged from 7 to 87 years with a mean age of 38.6years. The datas were studied under different headings. Site of fractures or dislocation [Table 1]: 208 (57.46%) patients had upper limb associated fractures or dislocation and154 (42.54%) patients had lower limb associated fractures or dislocation. Level of education of the study group [Table 2] 42 (11.6%) patients were not educated, 54 (14.92%) patients had passed eighth standard, 79 (21.82%) patients had passed tenth standard, 68 (18.78%) patients had passed twelfth standard, 119 (32.87%) patients had passed degree and above. Reasons for preferring treatment from native bone setter [Table 4] mostly due guidance from family/friends in 76 (20.9%) patients, due to socio cultural beliefs in 57(15.7%) patients, due to ignorance in 40(11.1%) patients, due to easy accessibility in 39 (10.7%) patients, due to affordability in 44(12.3%) patients, due to fear of hospitalization in 30(8.3%) patients, due to fear of Surgery in 55(15.1%) patients and due to fear of amputation in 21 (5.8%) patients. Complications presented by the patients after taking treatment from native bone setter [Table 5] mostly due to malunion in 138 (38.1%) patients, due to nonunion in 75 (20.7%) patients, delayed union in 19 (5.2%) patients, joint stiffness in 63 (17.4%) patients, pressure sore in 11 (3.0%) patients, due to neglected dislocation in 14 (3.9%) patients, due to compartment syndrome in 21 (5.8%) patients, due to Volkmann’s ischemia in 4 (1.1%) patients, due to chronic osteomyelitis in 8 (2.2%) patients and due to gangrene in 9 (2.5%) patients.
Table 1
Injury sustained
Table 2
Educational qualification
|
Education level |
Number |
Percentage |
|
None |
42 |
11.6 |
|
Upto 8th standard |
54 |
14.91 |
|
Upto 10th standard |
79 |
21.82 |
|
Upto 12th standard |
68 |
18.78 |
|
Degree or above |
119 |
32.87 |
Table 3
Source of contact
|
Source |
Number |
Percentage |
|
Neighbors |
112 |
30.93 |
|
Parents |
104 |
28.72 |
|
Friends |
79 |
21.82 |
|
Self |
54 |
14.91 |
|
Others |
13 |
3.59 |
Table 4
Reason for patronizing traditional bone setters
|
Reason |
Number |
Percentage |
|
Easily accessible |
62 |
17.12 |
|
Affordable |
84 |
23.2 |
|
Fear of Hospitalization |
48 |
13.25 |
|
Fear of Surgery |
78 |
21.54 |
|
Superstition |
68 |
18.78 |
|
Fear of amputation |
24 |
6.62 |
Table 5
Complications
Discussion
The study to evaluate why patients prefer native bone setters treatment and to identify common complications associated with it. The study was done from documented datas of 362 patients from a tertiary care hospital. In an era of accessibility to advanced orthopaedic care, native bone setters are still one of the largest group practicing traditional medicine in many developing countries. 1, 2, 3 Even in a country like ours with abundant of medical institutes and with the best advance medical care, about 60% of traumas are treated by native bone setters. 3, 4, 5 Mostly about 10-40% of patients around the world prefer ancient way of healing fractures. 1, 2, 3 In our survey of 362 patients, 221 were males (61.04%) and 141 were females (38.95%). The ratio of male to female was (1.56:1). Their ages ranged from 7 to 87 years with a mean age of 38.6 years. The study showed male predominance (221 males - 61.04%) as compared to females in other studies also. 8, 10, 13, 14, 15, 16, 17, 18, 19, 20, 21 Male preponderance were because male were more exposed to injuries, to traffic either as drivers or travelling to work and more active in rough and tough sports. In our survey mean age of patients was 38.6years which was noted in other studies too.22, 23, 24, 25 The study showed upper limb in 208 patients (57.46%) as most affected site of fractures and dislocation compared to lower limb in 154 patients (42.54%). In our survey we observed that educational status had no relation with preference of treatment selection as 119 (32.87%) patients had passed degree and above, similar observations were noted in other studies.2, 3, 4, 26 Reasons for preferring native bone setters treatment was first due to guidance of family/friends in 76 (20.9%) patients, second comes socio cultural beliefs in 57(15.7%) patients, third fear of surgery in 55(15.1%) patients, next comes affordability in 44(12.3%) patients, due to ignorance in 40(11.1%) patients, due to easy accessibility 39(10.7%) patients, due to fear of hospitalization in 30(8.3%) patients and finally fear of amputation in 21 (5.8%) patients. According to our survey family/friend was the most commonest reason for preferring native bone setters treatment which were similarly noted in other studies. 8, 16, 17, 27, 28, 29 And in some parts of Africa, socio cultural beliefs was the reason for preferring native bone setters treatment. 30, 31, 32 A study done in Northern Ghana, their observation showed the most common reason was superstition (37.5%), followed by affordability (31.25%) and easy accessibility (7.5%) for preferring native bone setters treatment.32In our survey we observed all the 362 patients have come to the emergency casualty or orthopaedic OPD after taking the initial treatment from various native bone setter. They all came with complains of continuous pain, discomfort and with difficulty in their movement. Another observation we noted in the study most of patients had presented within 10 – 14 days after taking initial treatment from native bone setters and a maximum of 3 years due to continuous pain and discomfort, increase joint stiffness causing increased difficulty in their movement. In our study, we observed the most common complications of the patients managed by the native bone setters were due to malunion in 133 (36.74%) patients, second due to nonunion in 69 (19.06%) patients and next due to joint stiffness in 58 (16.02%) patients, 21 (5.8%) patients had compartment syndrome, delayed union in 16 (4.41%) patients, 14 (3.86%) patients suffered from neglected dislocation, 11 (3.03%) patients had pressure sore, 9 (2.48%) patients developed gangrene, due to neglection 8 (2.2%) patients developed chronic osteomyelitis. Finally 4 (1.1%) patients developed Volkmann’s ischemia contracture. 33 Malunion and non-union were the most common complications of the patients managed by the bone setters which were similarly noted in most other studies. 10, 18, 22, 28 in another study showed stiffness of joint was the leading complication. 12, 21
Conclusion
In a country with abundant of medical institutes along with advance and best orthopaedic care present at the foot step. Without any relation to education or status, people still prefer native bone setters for musculoskeletal injury in urban area. This is because the people have confidence and strong belief in the abilities of the native bone setters which were mostly influence by family and friends, despite the complications associated with it. We should not forget, native bone setter’s practice played an important role of healthcare provider to the rural areas of our country. As we are orthopedic surgeons we want the people to stop believing blindly to myths and open their eyes to the reality regarding the adverse effects. According to our survey the scientific and also proper approach to solve this problem would be when our country’s health ministry take steps to evaluate and trained the native bone setters and educated the public, which will help to reduce the morbidity and mortality associated with complications related to native bone setter’s management.