Introduction
Spondylolisthesis is forward movement of one vertebral body relative to the adjacent vertebral body leading to instability, pain and other radicular symptoms.1 The most common site for spondylolisthesis is the lower lumbar spine at L5-S1 level with the forward translation of the L5 vertebral body over S1 vertebral body. The second most common site for spondylolisthesis after L5-S1 is at L4-5 level.2 Surgery may be the most appropriate treatment option when there is significant instability with neurological problems after the failure of all modalities of conservative treatment.
Posterior lumbar interbody fusion (PLIF) was done previously for achieving spinal fusion.3 This has been replaced now by Transforaminal lumbar interbody fusion (TLIF) developed by Harms.4 TLIF employs a posterior approach to fuse the anterior column of the spine and helps in disc resection, neural decompression, and circumferential arthrodesis in the lumbar spine.5 Though TLIF has been considered a safe technique with fewer complications compared to PLIF, considering fusion as a necessary pre-requisite for achieving optimal functional outcome remains a question of debate.6
This study aims at assessing the correlation between the functional outcome of the TLIF procedure with the fusion status of the patient through clinical and radiological evaluation of the patients between the preoperative and postoperative periods.
Materials and Methods
This is a retrospective study including 76 patients operated on between 2017-2019. Patients of single-level degenerative spondylolisthesis or isthmic spondylolisthesis who failed conservative care for 6 months were included. We excluded patients with previous spine surgery, trauma to the spine, or infection involving the spine. We also excluded patients of multilevel degenerative lumbar spondylolisthesis. Transforaminal lumbar interbody fusion with pedicle screw stabilization was performed in all the patients.
Data like VAS and ODI score measured before surgery along with their neurological outcomes were noted. Radiological data which includes anteroposterior and lateral flexion-extension view were utilized. MRI was used to measure the lumbar lordosis, slip angle and the grading of slip angle for all the patients included in the study.
Surgical procedure
The patient is positioned prone and through traditional midline approach appropriate lumbar spine was exposed. Pedicle screw stabilization was done under fluoroscopic guidance in the involved levels. Laminectomy was performed in patients with significant canal stenosis and on the side of the radiculopathy unilateral facetectomy was done. The disc space was made ready and a bean cage packed with autograft was placed. Lumbar lordosis was re-formed with the help of contoured rods. No attempt to reduce the spine manually was undertaken. Patients were mobilized after 48 hours with restricted bending and were instructed to restrict lifting weight post-operatively for 3 months.
Serial radiological evaluation and monitoring was done quarterly for one year period. Modified Lee’s criteria was used to measure radiological fusion.7 Radiological parameters such as slip angle, lordosis angle, and slip grade improvement were noted at the final follow-up. During the final follow up, the functional outcome was assessed with MacNabs’ criteria. Postoperative Visual Analog Scale (VAS) score and Oswestry Disability Index (ODI) scores were also recorded.
Statistical analysis was performed with SPSS software version 25. Students’ paired t-test and Pearsons’ correlation analyses were utilized for statistical analysis. P-value less than 0.05 was considered significant.
Results
We included only patients who completed one year of follow-up. The mean age of the population included for analysis was 53.4 years (SD=9.3). The M: F ratio was 45:31 with male predominance noted in the included population. Of the 76 patients included, 12 had an isthmic type and the rest all had a degenerative type of spondylolisthesis. Grade 3 spondylolisthesis was noted in 12 of the included patients while the rest all had Grade 2 spondylolisthesis. The mean surgical time was 90 minutes with mean blood loss being 350ml. L4/L5 remained the predominant level being operated. All the patients had a mean length of hospital stay of eight days.
The preoperative mean visual analog scale score for back pain was around 8.2 which was reduced to 2.1 at final follow-up which was a clinically significant improvement. A similar reduction was also noted in the VAS score for leg pain from 8 to 2.2 during final follow-up.
At the final follow-up, the preoperative ODI score of 72 was also reduced to 14 which showed clinical significance. The average slip angle was reduced from 24o to 6o. Although no attempt to reduce the slip grade was undertaken intraoperatively, a minimum one-grade improvement was noted in all the included patients. The mean cage size used in the cases was 10mm.
Of the 76 patients, 12 patients presented with neurological deficit. Sensory weakness was found in 8 patients and motor weakness was noted in 4 patients. All of them had improvement in their sensorimotor neurological status except 2 patients who remained the same as of preoperative status. 4 patients had a superficial infection which settled with appropriate antibiotics.
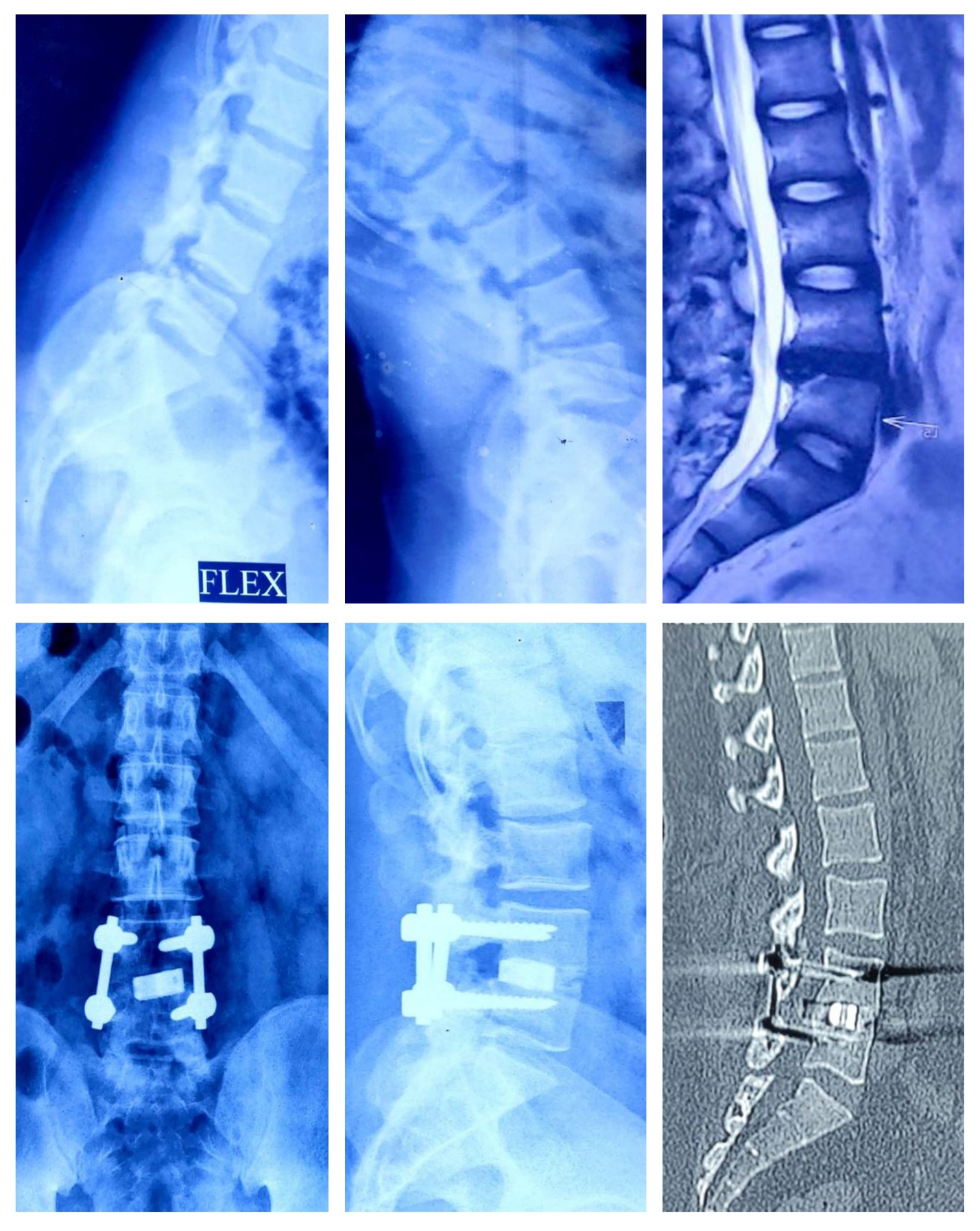
Lee’s criteria were used for Radiological evaluation of fusion and it showed definite fusion in 54 patients as shown in Figure 1, Figure 2 and Possible fusion was noted in 15 patients as shown in Figure 2. Whereas possible pseudoarthrosis was noted in 4 patient and definite pseudoarthrosis was found in 3 patients as shown in Figure 3. MacNab’s criteria was used to measure functional outcome and it showed excellent outcomes in 64 patients, good in 9 patients and fair in 1 patient as shown in Figure 4. Poor outcome was noted in 2 patients.
Correlation analysis between the pain scores and radiological fusion parameters analyzed (r=0.142, p=0.361) showed no significance. However, a significant correlation was noted between the fusion group and functional outcome parameters like the ODI score (r=0.34, p<0.001) and MacNab’s criteria (r=0.46, p<0.001).
Figure 1
llustrative case of grade 2 degenerative spondylolisthesis treated with transforaminal lumbar interbody fusion with pedicle screw stabilization

Figure 2
llustrative case of grade 1 degenerative spondylolisthesis treated with transforaminal lumbar interbody fusion with pedicle screw stabilization
Discussion
Spondylolisthesis is the most common cause of lower back pain which is due to the anterior displacement of the vertebral body about the bordering vertebral bodies. Nerve root compression presents as radiculopathy in Spondylolisthesis.2, 3 Conservative or surgical management of spondylolisthesis depends on the grade and functional disability on the patient’s routine. Surgical treatment for spondylolisthesis includes decompression followed by instrumented fusion which comes into action after treating conservatively with rest, pain control, and bracing.5
Myerding classification describes five grades of spondylolisthesis depending on the vertebral slippage amount on radiographs about the caudal vertebrae. Grade I includes less than 25 percent slippage, grade II 26–50% slippage, grade III is 51–75% slippage, grade IV being 76–100% slippage, and grade V is over 100% slippage.6
Patients with grade I and grade II spondylolisthesis can be treated conservatively, whereas, surgical management remains questionable for patients with grade III, IV and grade V spondylolisthesis,. Harris et al. compared grade III and IV spondylolisthesis patient who had been managed surgically and conservatively and proved no significant difference between the two groups.8 Lundine et al. also had similar findings with grades III, IV and V spondylolisthesis patients.9
Harms developed the TLIF procedure as an alternative to traditional posterior lumbar interbody fusion (PLIF).The advantage of TLIF is successful fusion without the risk of nerve root tethering, which is a common complication with traditional PLIF techniques. Besides, TLIF eliminates epidural scarring and less surgical time which helps in reducing intraoperative bleeding.10
In TLIF, surgical hardware is applied posteriorly to the fasten fusion rate. Bone graft and interbody spacer stabilize the anterior portion of the spine whereas the pedicle screws and rods are attached to the back of the vertebra. It fuses the vertebra above and below as the bone graft heals.11 The VAS and the ODI are commonly used scales to assess patient-reported outcome measures in spinal deformity patients.12 According to Houten et al. study on 33 TLIF-treated patients who were followed with investigations over a period of 37 months, their functional scores improved from 4.9 to 7.13
Poh et al. study on the two-year outcome of TLIF concluded that all elements of the SF-36, the VAS scores which explains pain level, and the NASS scores enhanced significantly after TLIF with p value less than 0.01.14 Lauber et al. study demonstrated that the median ODI in degenerative spondylolisthesis patients reduced from 23.5 to 13.5 points and in isthmic spondylolistheses patients, it got decreased from 20.5 to 10.95 after 2 years.15 Foley et al.in his study have showed that the ODI score got decreased from 55 before the operation to 11 after the operation.16 Similarly, the VAS score for leg and back pain improved significantly after TLIF in our study. ODI score also showed statistical significance compared to the preoperative period.
The intervertebral foraminal area increased by 45.5% after transforaminal decompression and the intervertebral foraminal area increased by 34.2% after the posterior decompression according to Osman et al.17 Hackenberg et al. showed the success rate of bony fusion of transforaminal lumbar interbody fusion to be around 86%.18 According to Kim et al. the disc space height and the whole lumbar lordotic angle during the radiological evaluation increased at the final follow-up and the radiological union was obtained in 95.4% of the cases.19 Femke et al. study recorded that non-union and loss of reduction radiographically did not affect the clinical outcome.20
According to a study by Audat et al, there was no significant correlation between reduction and clinical outcome. The study included 41 symptomatic low-grade spondylolisthesis patients who underwent posterior lumbar interbody fusion (PLIF) with reduction and fusion in-situ.21 A retrospective multicenter clinical study by Thalgott et al. concluded that the fusion rate was consistent with the clinical outcome.22 Although our study showed no significant correlation between the pain parameters such as VAS scores of back pain and leg pain, a significant correlation was noted between fusion and the functional outcome among the included patients.
Our study has certain limitations. First, the retrospective nature of the study design would not evaluate all the potential preoperative parameters which would have altered the decision of the surgery. Second, the limited sample size of the study done in a single institution would not allow us to generalize the result of the study to the general population. Hence we recommend a large multicentric randomized controlled trial to further validate the findings of this study.


