Introduction
Anterior cervical discectomy and fusion (ACDF) was first introduced by Bailey-Badgley,1 Smith-Robinson and Cloward2, 3 in the year 1950 and early 1960.
For the treatment of neoplastic, traumatic, degenerative and other cervical pathological conditions - the anterior approach is highly preferred. The approach has the advantage of being safe and easy for soft tissue dissection, good visualization making easy removal of soft tissues and low rate of associated complications. Though there are minor technical complications of this approach but the most concerning complication is pseudarthrotic segmental healing, fracture due to graft compression, kyphotic segmental deformations and dislocation of graft. Anterior plate placement to the segment being treated has shown positive results in reducing these complications. However, there were still few complication related to implant like breakage of screw, plate and loosening of screw by using this surgical technique. The literature stated the reason for this complication as the loosely attached screws for which a rigid plate designs was developed with firmly attached screws. The rigid plate design provided firm mechanical fixation to the segment and help in rapid healing of bone. The use of anterior plates has provided promising results in significantly reducing complications like, resorption of graft, compression fractures of graft, graft dislocation leading to pseudarthrotic healing and kyphotic angulation.
Anterior cervical decompression along with inter-body fusion is widely accepted and gained popularity amongst the spine specialty for managing variety of diseases, which can be categorised as under degenerative disc disease, traumatic conditions, tuberculosis, tumours and miscellaneous.
Aims and Objectives
To study the efficacy of fusion with anterior cervical discectomy, iliac crest bone grafting with or without fixation with anterior self locking titanium cervical plates.
To compare the outcomes in instrumented vs. non-instrumented anterior cervical fusions in terms of post-op symptom relief and neurological improvement.
To study complications in these patients.
Materials and Methods
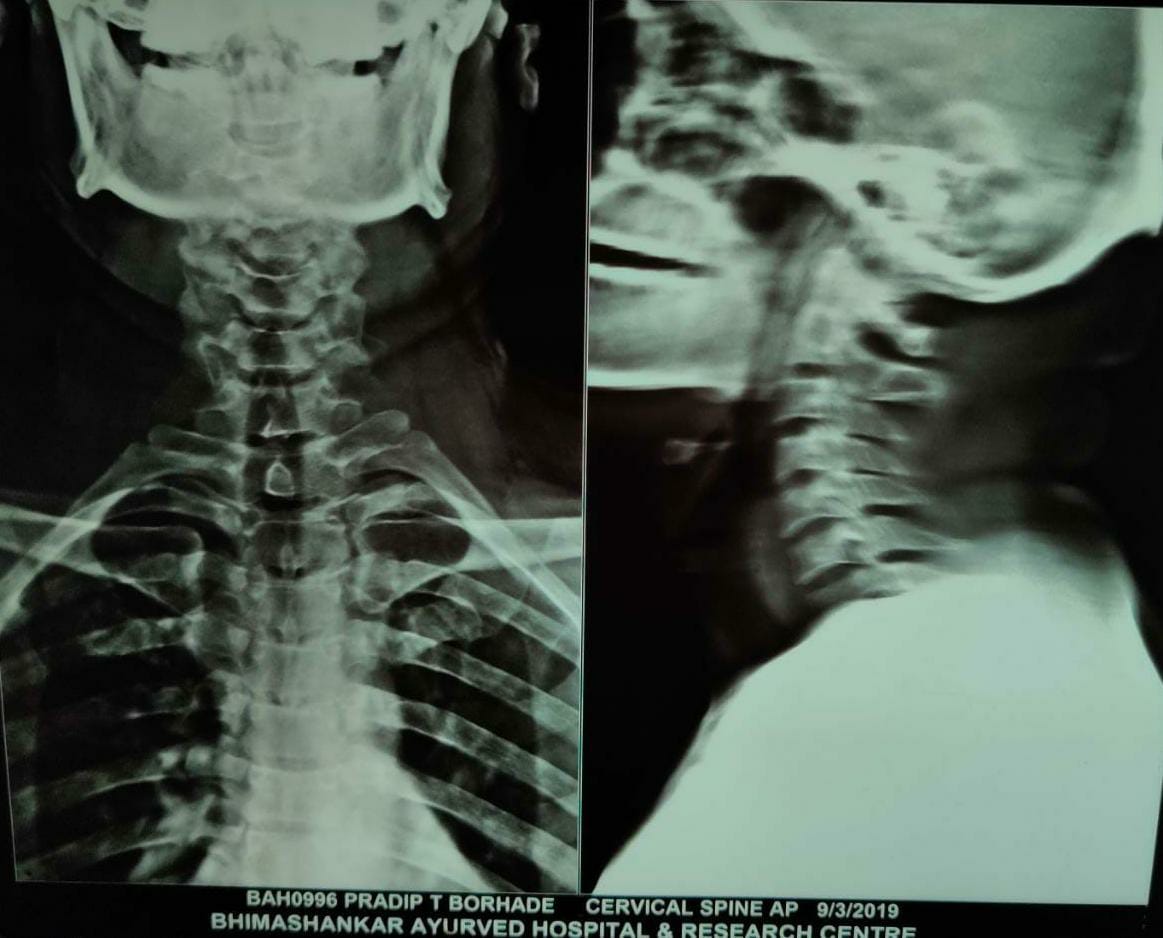
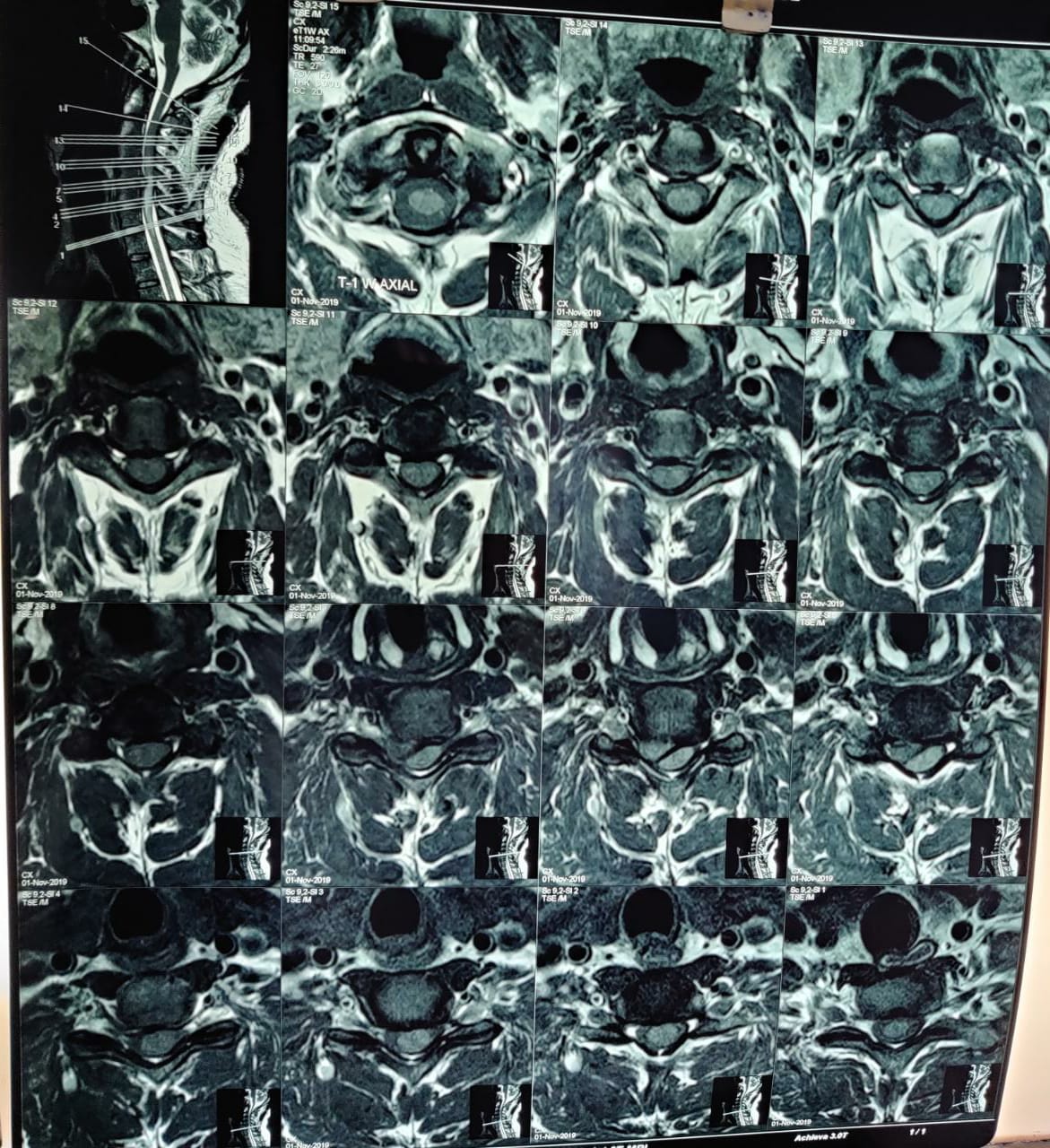
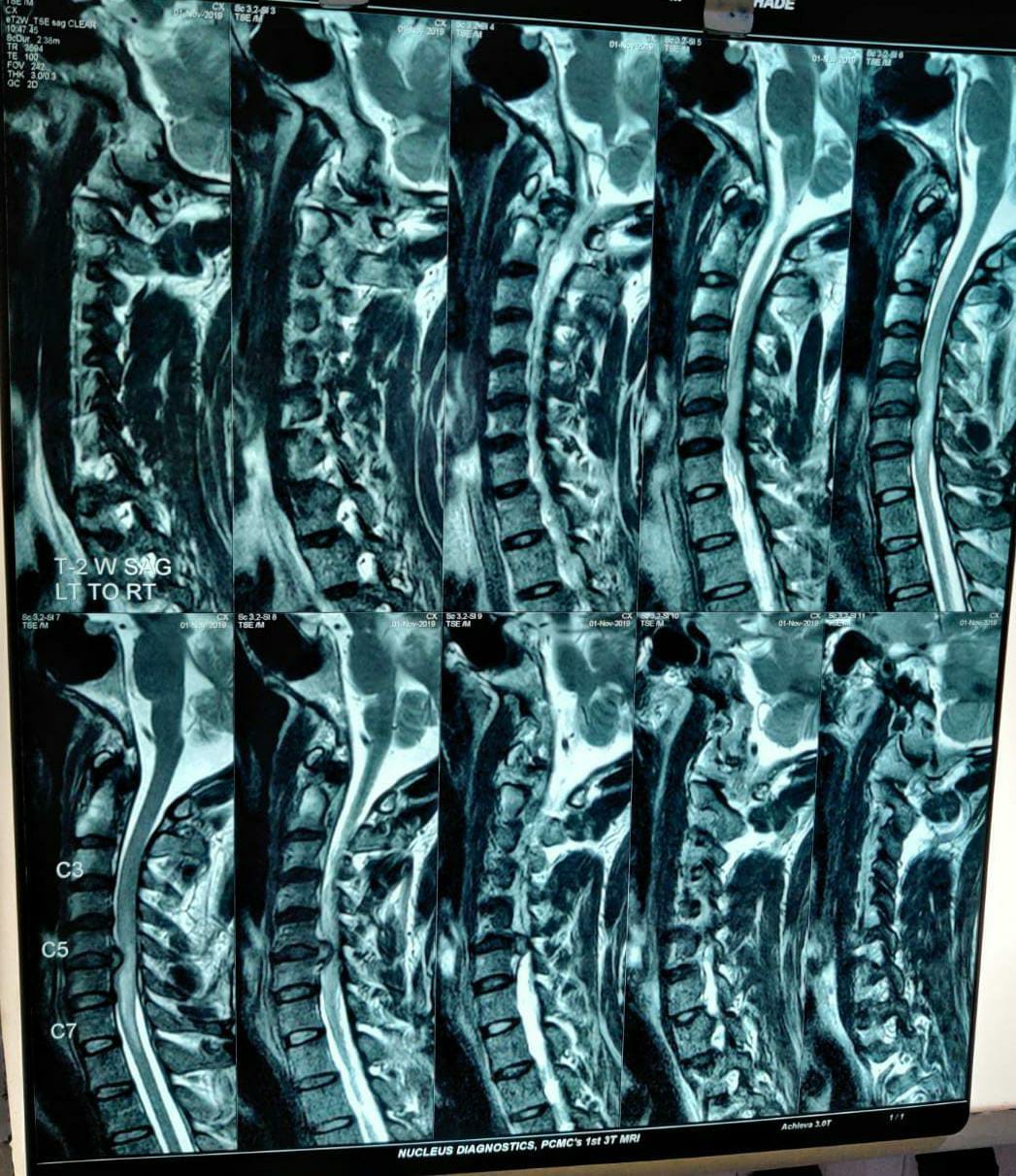
A prospective study of 20 cases of anterior cervical interbody fusions done in our Institute, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune, between June 2018 to August 2020 with a follow-up period of 6 months was done.A detailed history and clinical examination was done according to a specified performa. Radiographs, MRI and other relevant investigations were done. A detailed neurocharting was maintained on admission, post-op, weekly thereafter for 2 weeks and monthly thereafter was done. A written informed consent in the language known to the patient was taken after explaining the details of the surgery and the risks of complications, morbidity and mortality associated with the same.
Inclusion criteria for degenerative disc disease
Patients with frank myelopathy, patient with a progressive neurological deficit, patients with a static neurological deficit with having unremitting pain, failure of conservative management or non-operative treatment taken for at least three months in the absence of any acute neurodeficit.
Exclusion criteria
Cervical disc disease with symptoms less than 3 month’s duration in the absence of acute neurodeficit and previous cervical spine surgery.
Surgical approach
Identify the landmarks and draw a transverse incision that extends from the midline to the middle of the sternocleidomastoid muscle. Create a plane undermining the skin and subcutaneous tissue superiorly and inferiorly. Divide the platysma in line with skin incision followed by division of deep cervical fascia. Identify the left recurrent laryngeal nerve and mobilise the carotid sheath laterally and trachea and oesophagus medially. Once the vertebral layer is exposed, the level is confirmed using a prebent needle under C-arm guidance.
The level is identified and necessary discectomy is performed until the posterior longitudinal ligament is visualized. Using a burr, end plates are cleared off any anterior osteophytes. Decompression of spinal cord and nerve roots done. Interbody graft placed with anterior cervical plate fixation in necessary cases.
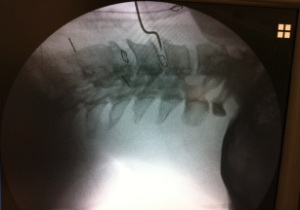
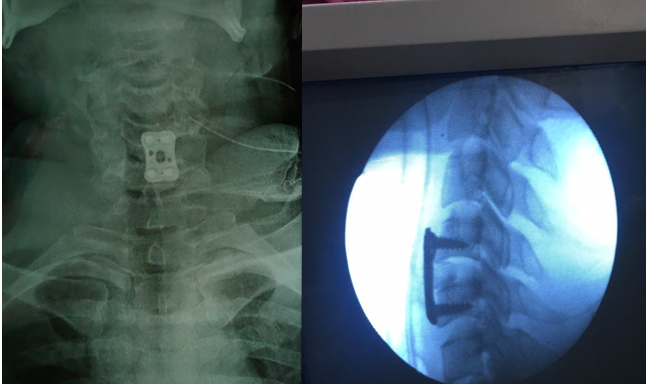
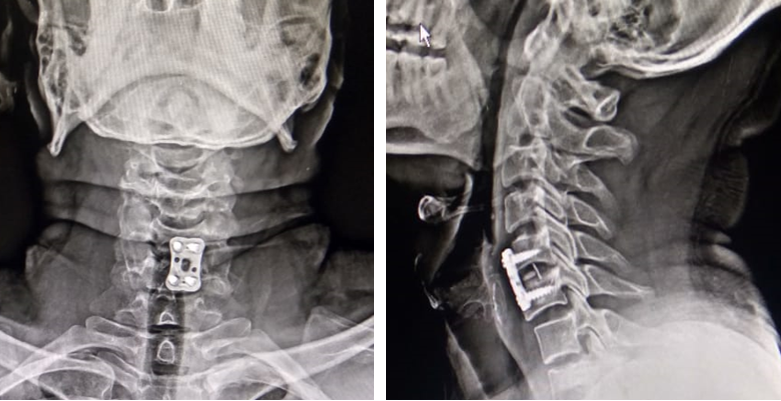
Case 2
30 year old male with cervical myelopathy due to C5-6 disc bulge (single level non instrumented fusion).
Observations and Results
In all, 20 cases of anterior cervical fusion for various indications were included in this study. Of these, 6 were for traumatic indications, 13 were degenerative radiculo / myelopathy and 1 was tuberculosis. Most patients of the degenerative group were in 41-60 age group(6/13 or 46.2%), while most among the trauma group were in 21-40 age group(4/6 or 66.7%).
Table 1
Age distribution of patients in the study was as follows
|
Age of Patient |
Trauma I |
Trauma NI |
Degen I |
Degen NI |
Others I |
Others NI |
|
0-20 |
0 |
0 |
0 |
0 |
0 |
0 |
|
21-40 |
3 |
1 |
2 |
2 |
0 |
0 |
|
41-60 |
1 |
1 |
2 |
4 |
0 |
0 |
|
>60 |
0 |
0 |
2 |
1 |
0 |
1 |
|
Total |
4 |
2 |
6 |
7 |
0 |
0 |
Table 2
Sex distribution was as follows
|
Sex |
Trauma I |
Trauma NI |
Degen I |
Degen NI |
Others I |
Others NI |
|
Male |
2 |
1 |
5 |
7 |
0 |
0 |
|
Female |
2 |
1 |
0 |
0 |
0 |
1 |
|
Total |
5 |
2 |
5 |
7 |
0 |
1 |
Thus, 14 (70%) were single level fusions, 5(25%) were 2 level fusions and 1 case (5%) of 3 level fusion was included. All the multi-level fusions in this study involve corpectomies.
Table 3
Number of levels fused
|
No of levels |
Trauma I |
Trauma NI |
Degen I |
Degen NI |
Others I |
Others NI |
Total |
|
Single |
2 |
1 |
3 |
7 |
0 |
1 |
14 |
|
2 level |
3 |
0 |
1 |
1 |
0 |
0 |
5 |
|
3 or more |
0 |
0 |
1 |
0 |
0 |
0 |
1 |
|
Total |
5 |
0 |
5 |
8 |
0 |
1 |
20 |
Thus, 9 out of 14 single level fusions were at C5-6 level(64.3%). Among degenerative cases, 3 out of 5 single level fusions were at C5-C6 level(60%).
Table 4
Anatomic levels of single level fusion
|
Anatomic level |
Trauma I |
Trauma NI |
Degen I |
Degen NI |
Others |
Total |
|
C3-4 |
0 |
0 |
0 |
1 |
0 |
1 |
|
C4-5 |
0 |
0 |
1 |
0 |
0 |
1 |
|
C5-6 |
3 |
0 |
1 |
5 |
0 |
9 |
|
C6-7 |
1 |
1 |
1 |
1 |
0 |
3 |
Table 5
Early post-operative complications
Table 6
Frankels grading
|
Frankel’s Grade |
Pre-operative I |
Post operative I |
Pre-operative NI |
Post-operative NI |
|
A |
2 |
1 |
0 |
0 |
|
B |
0 |
2 |
2 |
0 |
|
C |
5 |
1 |
5 |
2 |
|
D |
2 |
3 |
3 |
4 |
|
E |
1 |
3 |
0 |
4 |
Thus, 70% (14) of the total cases ended up with a usual post –op neurological function(Frankel’s Grade D/E).
As shown above,18(90%) patients went on to solid fusion at the end of follow-up. One patient has been labelled here as doubtful, as the radiological signs were not seen at 12 months follow-up which was the maximum follow up that patient had.
Table 8
Speed of fusion
|
|
At 6th month |
At 9th month |
At 12th month |
At 18th month |
Total |
|
I |
7 |
2 |
1 |
0 |
10 |
|
NI |
5 |
3 |
0 |
0 |
8 |
As we see here, 7(70%) of the patients who were plated showed fusion at 6 months follow-up, as compared to 5(62.5%) out of 8 non-instrumented patients who showed fusion at 6 months.
Table 9
Outcome
|
Outcome |
Instrumented |
Non Instrumented |
Total |
|
Excellent |
1 |
1 |
2 |
|
Good |
4 |
5 |
9 |
|
Fair |
1 |
1 |
2 |
|
Poor |
0 |
0 |
0 |
The Table 9 shows that 11(84.6%) out of 13 patients in their degenerative group showed good to excellent results. No significant difference was seen between plated and non-instrumented groups as far as clinical outcome was concerned. The harvesting of autologous bone graft caused a transient morbidity with at the donor site haematoma in 25% of the cases.
Radiological outcome assessment
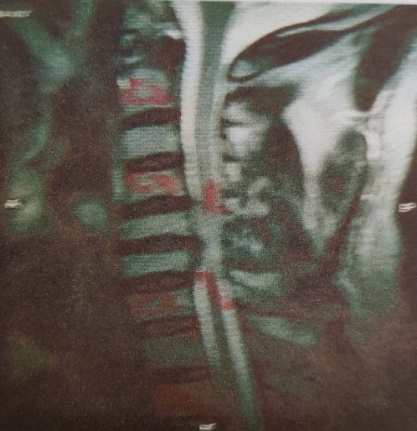
Anteroposterior as well as lateral cervical spine radiographs were routinely obtained at 3 months, 6 months and a year after the medical procedure and contrasted with preoperative X-rays to distinguish changes in shape and position of the cervical spine and in the placement as well as form of bone graft, and to search for indications of a bony fusion. A strong fusion was affirmed when rigid trabeculae were found in the utilized intervertebral space. Non-union was characterized as a bone's failure to form bridge of trabaculae across disc space. The collapse of the graft was considered if in excess of 3 mm loss of height were found in the later postoperative radiographs after a year. If there was more than 3 mm displacement then it was termed as dislocated. If there was loss or reverse of physiological cervical lordosis then it was diagnosed as postural abnormality. The vertebral bodies that were adjacent to level of fusion were extended on a radiograph by drawing line. Following this, the angle between these lines was measured as a intersegmental angle.
Loss in the normal alignment of cervical spine post-fusion in the form of segmental kyphosis or simply loss of lordosis was seen in 2(10%) of the patients, both of which were non-instrumented as shown in the table below.
Long term subjective satisfaction
In degenerative group, 9 patients (69.2%) were most satisfied with the results, 2 patients were satisfied (15.4%), and 2 patients (15.4%) were not satisfied with the long term results. Out of the 13 patients, 9(69.2%) resumed working in the same job, 2 (15.4%) initiated other jobs, 1 (7.7%) patient was unable to work, and 1 (7.7%) patient was permanently disabled.
Neuroradiological Findings at 1 Year after Surgery
18 patients (90%) showed a normal shape of the cervical spine after surgery. In 1 case, there was a lessening or loss of cervical lordosis, and in 1 patient there was an antilordotic cervical spine with kyphosis angles. In none of the patients with irregular cervical spine position, the deformation related with diligent or transitory neck torment.
In 5%, lateral xray displayed a collapsed graft. In 5% the graft was dislocated anteriorly. Concomitant symptoms and signs were not observed.
1 of the patients showed presence of pseudarthrosis, however nobody had extreme pain in the neck or required surgical revision.
Discussion
The soft tissue dissection has proved to be safe and easy. It provides a direct view of anatomical structures. Thus there are less reported rates of complications. For the management of pathological conditions like neoplasm, trauma and degeneration, the ventral approach is preferred. Usage of anterior plates has reported significantly reduction in compression of surgical graft, dislocation, resorption of graft and compression fractures. The spinal stability is immediately enhanced by doing plate fixation. Along with this it also improves rate of one fusion, decrease in the reuirement of externanl immobilization.
In cervical spine degenerative disease, anterior approach to the spinal canal is more attractive and rational operative strategy because spondylotic compression occurs anteriorly. Likewise anterior approach has low rate of significant complexities and morbidity post operative. This approach also has a high degree of success of reliving of symptoms. The introduction of plate fixation has lead to improvement in stability, reduction in rate of pseudarthrosis, maintaining cervical lordosis and improving the associated clinical outcomes. A study reports 90% fusion rate wherein the surgery is conducted with or without internal fixation.
Our study included 13 patients of degenerative cervical spine disease.Most patients of the degenerative group were in 41-60 age group(6/13 or 46.2%). From these,single fusions were 10, two level fusions were two and four level fusion was one. All multi level fusions in this study involved corpectomies.
Our report demonstrates the efficacy of procedure and the adequal decompressionmyeloradiculopathy was significantly improved in 84.6% of cases. Our data good long term results are within the range of Myeloradiculopathy as described below.
The results of the study reporting cervical myelopathy treated with anterior dissections followed by fusion using autogenous bone graft are like-Wiberg4 in1986 reported that good results were found in 80% cases,
Bernard and Whitecloud5 reported 76%, while 78% were observed in Irvine and Stachan in 1987, 50% in Probst6 study in 1989, 70% in Senter et al reported in the year 1989, 50.4% in Yonenobu7 et al. in 1991, 60% in Jacchia et al. reported in the year 1992, 51% reported in the year 1993 by Arnold8 et al. and 90.9% good results reported by Gaetani et al. in the year 1995. In the present study, the percentage was highest i.e., 84.6%.
Traumatic cervical spine disease
Operative treatment is required in case the injuries of cervical spine are with or without the neurological defect. The early functional rehabilitation and stability is enhanced by open reduction and internal fixation technique. Any of the approach whether it is posterior, anterior or a combination of both can be concerned for stabilization of fractures of cervical spine. Healing via this procedure occurs within 8-12weeks and thus it allows mobilization of the patient quickly.
We had 6 patients of cervical spine trauma in our study. Most among these, especially burst fractures required corpectomy with 2-level discectomy and fusion.
The anterior decompression and strut grafting done in the posterior fractures that are unstable then it leads to recurrent deformity along with instability. The steps should be always in a sequence of; firstly, obtaining posterior stability; secondly, anterior decompression and thirdly, fusion is done if indicated.
When the injuries of the spine involves facets, subaxial cervical spine, articular pillars and posterior ligament then posterior approach is considered and it becomes essential fuse one cervical segment of cervical motion. There is less blood loss when anterior approach is followed. Moreover, the stabilization of injuries is possible with only fusion of one motion segment while in case of posterior approach, there is a need for fusion of two motion.
Early post-operative complications in our study included complications like haematoma and pain at the donor site of graft. These complications were seen in 25% as compared to 20% in the literature.
Infection at the donor site of graft and lesion on the lateral cutaneous nerve was not reported in any patients. Schnee 9 et al. in the year 1997 reported 5.6% patients having disturbance in healing of wound, 2.8% with post operative pain necessitating surgical re exploration. But confounding factors were the disproportionate numbers of obese patients, women and patients with medical complications. 25.3% morbidity and 17.3% pain at graft donor site was observed in the study reported by Sawin et al.10 in the year 1998.
Options to avoid these complications are: anterior cervical discectomy without grafting or use of allograft. In order to prevent loss of cervical spine sagittal alignment, to prevent loss of height of disc, to reduce pain in the neck and to prevent narrowing of foramina, a fusion following anterior cervical discectomy must be done. When pseudarthrosis and rate of graft collapse are compared then a higher rate are given by allograft over autograft. (An et al. 1995).
Other early complications were temporary unilateral lesion of recurrent laryngeal nerve causing dysarthria in 10 percentage of our patients, and deteroration of neurological deficits in 10 percentage. The reported incidence in the literature for recurrent laryngeal nerve is 1-11%. The reasons for these complication are stretch injury, injury due to thermal necrosis, traumatic division, and compression due to postoperative swelling. It becomes impossible to close the larynx completely and thus risk of aspiration increases. Moreover the voice becomes hoarse and weak. Prolong presence of symptoms beyond 6 months necessitates a referral to otolaryngologist.
Our study shows neurologic deterioration in the early post operative period in 10% cases. 5.5% rate of myeloradiculopathy was reported by Yonenobu et al in the year 1991, the rate was 11.4% in Arnold et al. study conducted in 1993. After decompression, patients deteriorated post myelopathy surgery. The factors which determine the surgical outcomes include, whether it is a soft or hard disc pathologic condition, presence of post operative symptoms and the age of the treated patient.
The major complications observed post anterior cervical fusion are non-union and dislocation or collapse of graft. Our study showed 18(90%) patients going on to solid fusion at the end of follow up. One patient has been labelled as doubtful, as the radiological signs were not seen at 12 months follow-up which was the maximum follow-up that patient had. Nevertheless his clinical outcome in terms of neuro-recovery was good. Inspite of using autograft, the non fusion reported rate are between 3-7% for single level fusion. The rate is 12-18% for two level fusion by using autogenous iliac tricortical graft. Similar is noted for three as well as multiple level fusions. As reported by Wang et al, the rates are significantly reduced by the use of two-level anterior cervical discectomy and fusion. Madawi et al.11 in the year 1996 conducted a study of 115 patients. The patients were treated with osteoconductive polymer implants. The long term outcomes, complications, radiographic outcomes ad stay in hospital were the parameters assessed. In 74 patients, the Smith-Robinson technique was used while the Cloward technique was done among 41 patients. The clinical outcome in both the treated groups was same. A significantly higher proportion for intersegmental kyphosis post operatively and partial graft protrusion was reported with the patients treated using iliac bone graft as compared to the ones treated with polymer graft. In Zdeblick and Ducker study reported in the year 1991, data on 87 patients undergoing Smith Robinson anterior fusion was discussed. When the comparison was made between Tricortical allograft iliac crest bone and tricortical autograft, the proportion of delayed union were more in allografts as well as two level fusion procedure. Both the groups likely reported for relief from neck and arm pain. Comparison of autograft with allograft was doe in one of the study by Fernyhough et al.12 in 1991. The outcomes reported an increase in the union rate with increase in the quantity of motion segments fused. Similar was reported by Emery et al.13 in 1997 with a high pseudarthrosis rate by doing three level modified Robinson cervical fusion. The conclusion provided by most of the authors was that, a successful bony fusion will always have a improved result.
The results of the present study are not in concordance with the statement that the clinical outcomes significantly correlates with the radiographic outcomes. But correlation is definitely reported by other authors. A correlation was found between collapse of graft, unfavorable clinical outcomes and posterior kyphosis.
Anterior cervical plating improves the rate and speed of fusion, and also prevents loss of the sagittal alignment of cervical spine, as compared to non-instrumented fusions, which is supported by the literature.
Conclusion
Anterior cervical fusion is an efficacious procedure for cervical myeloradiculopathy, traumatic and other indications where anterior decompression is warranted, with good to excellent outcomes in majority of cases.
Anterior cervical plating helps achieve fusion faster when compared with non-instrumented fusion, with decreased need and period of external immobilization.
Plating also prevents to some extent loss of sagittal alignment of cervical spine, when compared with non-instrumented fusion.
Plating also decreases the rate of complications like pseudarthrosis, graft collapse, dislodgement etc.
Hence, we strongly recommend plating in all anterior cervical fusions, especially so in