Introduction
A mallet finger occurs due to injury to extensor tendon terminal insertion or rupture of extensor tendon or it may be caused by avulsion fracture of dorsal base of distal phalynx,1, 2, 3 Commonly these injuries are treated conservatively using an immobilization splint that immobilizes the Distal interphalangeal joint (DIP) for 6-8 weeks.4 A mallet fracture is a bony mallet finger which happens due to avulsion fracture of dorsal base of distal phalynx.5 Most commonly it happens during sports which involves catching a ball, commonly in small, ring and middle finger,5, 6 with mechanism of injury being sudden forced DIP flexion along with axial loading on long axis of the digit.5 A bony mallet can be treated conservatively if the fracture is small and involves less than a third of articular surface.7 If the mallet fracture involves greater than 30% of articular surface, with volar subluxation and articular stepup greater than 2 mm and in patients in whom it is hard to do immobilization, surgical treatment is warranted.8 While many surgical techniques have been described in literature, ISHIGURO introduced the extension block pinning method which is very simple, easy to perform and gives good clinical outcome.9 In this study we intended to evaluate the efficacy of Extension block pinning for the management of Mallet fracture.
Materials and Methods
This study was done in 15 patients from year 2018 to 2020,Tendon injuries, open injuries are excluded from the study. Mallet fracture involving greater than one-third of articular surface, joint subluxation, greater than 2 mm step off of fragments was included in this study. This study included 13 males, 2 females with a mean age of 33(range 18-50) with 8 ring finger, 2 middle finger, 5 little finger. All the patients are operated within 2 days of injury. The mallet fractures were classified using wehbe & Schneider classification (Table 1).
Table 1
Wehbe and Schneider classification of mallet fractures
|
Type of fracture |
Description |
Subtype |
Articular involvement |
|
1 |
No DIP joint subluxation |
A |
<1/3 |
|
2 |
DIP joint subluxation |
B |
1/3-2/3 |
|
3 |
Epiphyseal and physeal injuries |
c |
>2/3 |
12 patients had mallet fracture type 2b, 3 patients had type 2c. All the patients were followed up for a minimum of 4 months and results were evaluated using Crawford criteria (Table 2).
Table 2
Crawford’s criteria for evaluation of mallet fracture treatment
Surgical technique
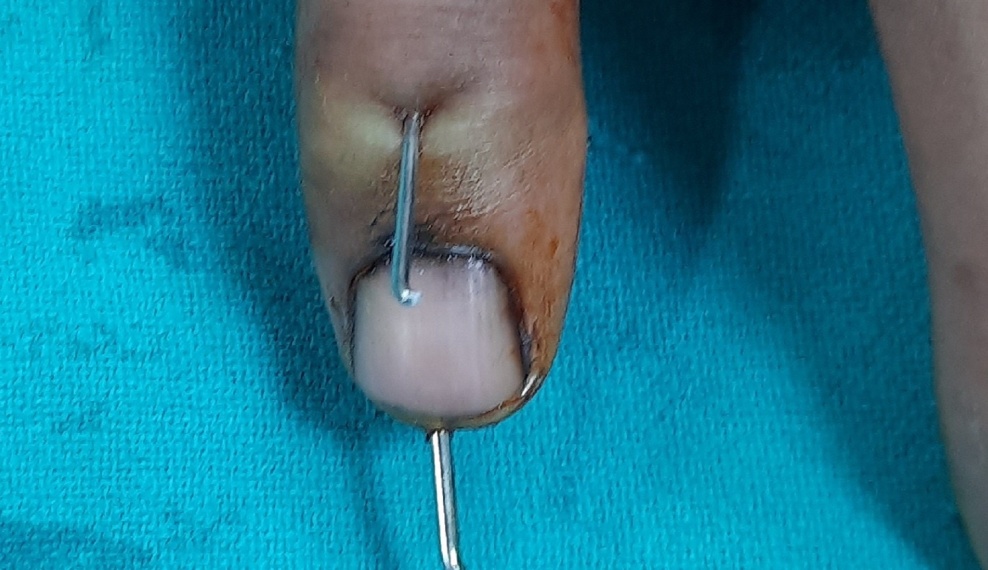
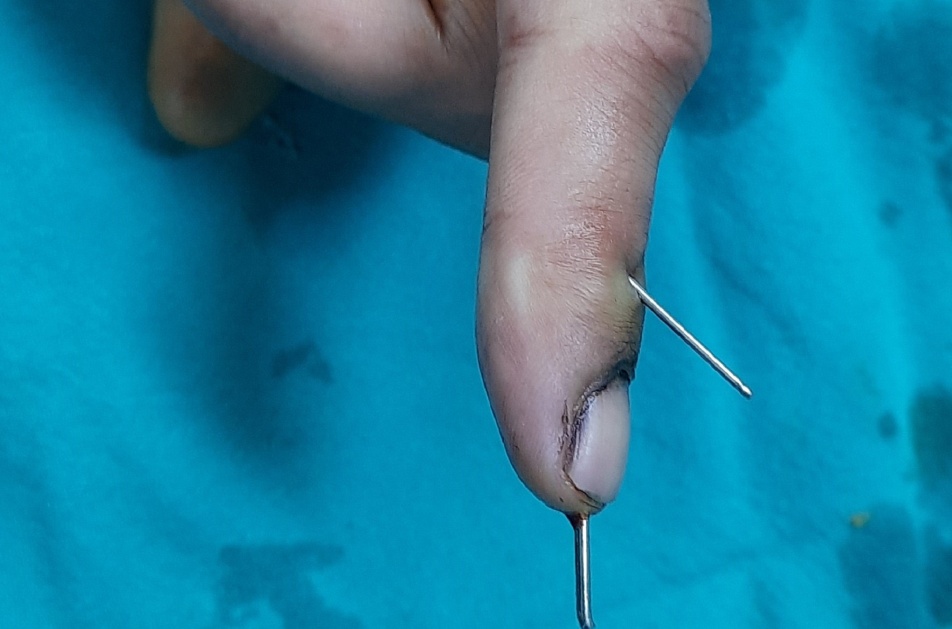
The surgery was done using digital block anesthesia, c-arm is used during the surgery, no tourniquet is used. The DIP joint is held at 80o flexion, then a 1 mm k-wire is passed just proximal to the Prominent Dorsal DIP joint crease at an angle of 45o to catch the terminal extensor tendon, just behind the dorsal fragment leaving ample room for another transarticular k-wire.
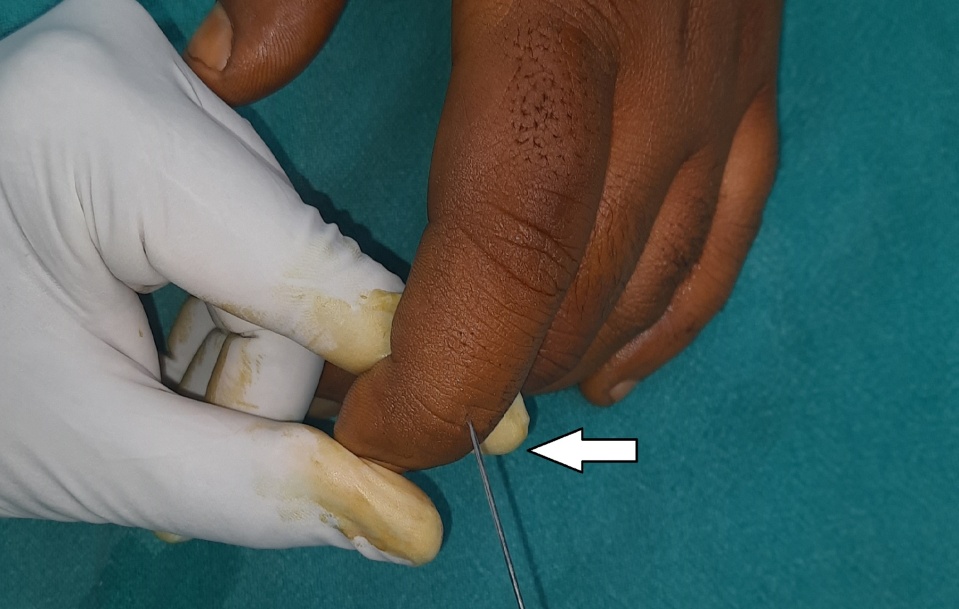
Then the DIP joint is brought into full extension, reduction is confirmed using c-arm, then with DIP joint in slight hyperextension another 1 mm k-wire is passed through distal phalynx across DIP joint into the head of Middle phalynx. Then the final c-arm checking is done, wires were bent, and final dressings was done.
Figure 6
Showing placement of Extension block pin 3 mm proximal to prominent Dorsal DIP joint crease with DIP joint in 70 degree flexion and pin at a angle of 45 degree
No splint was given. The PIP joint movement is encouraged from day one.the wires were removed at 6 weeks as OPD procedure and active DIP joint mobilization started with a night splint for further two weeks, after 8 weeks unrestricted movements are allowed.
Results
Results were calculated at the end of 4 months using Crawfords evaluation criteria, preoperatively the patients had a mean extension lag of 23o(Range 10o-32o), post-operative extension lag improved to a mean of 3o (Range 0o-5o), the post op flexion of DIP joint was at a mean of 78o(range 70o-80o).
All patients were painfree, none of them had any pintract infection or skin maceration, According to Crawford criteria ten patients had excellent results, 5 patients had good results.
Table 3
Discussion
Acute mallet finger that occurs as a result of extensor tendon rupture (or) involving less than one third articular surface can be treated with volar splint that keeps DIP joint in extension, here the splint should be worn for 6 weeks continuously followed by a night splint for another 2 weeks.
Skin care is of utmost importance during conservative treatment as continuous splint may lead to skin maceration and ulceration.10
The mallet fracture occurs in 5-10% of mallet finger.11, 12
Jain D et al. in their series of 19 cases obtained 11 excellent results, 4 good result and 4 fair outcomes, One case had superficial pin tract infection. In our series we had 10 excellent results and 5 good results. We did not had any pin tract infection, we attribute this to the patient education of pin tract management.13 Ricardo M et al. in their series of 10 patients reported 3 excellent results, 6 good results, and 1 had fair result. In our series we had 10 excellent results.14
A mallet fracture which involves greater than 1/3rd of articular surface needs surgical intervention for maintaining anatomical reduction and to prevent extension lag.9 Many surgical technique have been described in literature eg (screws, pullout wire) but they are crumber some and difficult to perform in a small fragment.
The extension block pinning technique introduced by ishiguro et al is a simple, yet effective, and easy to learn and perform and it achieves a good anatomical reduction and gives excellent results and gives better results in acute cases.15
Ishiguro et al recommend a 18g needle to fresher fracture surface in cases older than 2 weeks before passing an extension block pin.15
A large mallet fracture (>1/3rd articular surface) may be due to a hyperextension and impact loading forces,16 may lead to DIP joint subluxation (>48% of articular surface) due to absence of stabilizing effect of extensor tendons (or) collateral ligament,17 moreover, a large fracture fragments may give difficulties in anatomical reduction, rotation, these difficulties can be tackled by a judicious use of transfragment k wire (or) two extension block pinning method.18, 19
In our study, we did not encounter any pin related complication and skin maceration, this may be attributed to proper education of patient about pin tract dressings and importance of keeping the skin clean and daily dressings.
The DIP joint have multiple dorsal creases, the prominent crease will lie over the DIP joint when the DIP is flexed to 80o, in our study we attempted to pass the extension block pin 3mm proximal to the prominent DIP joint dorsal crease at an angle of 45o, in all 15 patients we were able to place the extension block pin in Middle phalanx head. This finding have not been reported previously in the literature.
Technical tips to be remembered while considering Extension block pinning includes.
Gently Milk the middle phalynx distally before flexing the DIP joint.
Aim Your extension Blocking Pin 3mm proximal to the dominant DIP joint Dorsal crease, at an angle of 45o, leaving space for the next pin.
Hyperextend the DIP joint before placing the transarticular pin across DIP joint.
Avoid Hyperflexion of the DIP joint while passing the Extension block pin, as this may cause the thin terminal extensor tendon to get stretched in the long run and this indirectly contribute to extension lag after pin removal.
If avulsed fragment is very large(>2/3), and creates difficulty in anatomical reduction, a transfragmental wire is passed before extension block pin.18
If a large (>2/3) anatomically reduced fragment is unstable due to rotation, then a two –extension block pinning is done, leaving space for transarticular pin.19, 20.
Advice a night splint for two more weeks after kwire removal to prevent passive injuries during sleeping.
Teach the patient how to do pin care and daily dressings.
Conclusion
Based on this study we conclude that extension block pinning is an easy to perform and effective option for acute mallet fracture and gives very good functional outcomes, strict adherence to technical details and patient education regarding pin tract care is essential to achieve good outcome.