Introduction
Spinal tuberculosis is the commonest form of skeletal tuberculosis, accounting 50% and mainly involves the thoracolumbar and thoracic region.1, 2 Lumbosacral junction represents an uncommon site for tuberculosis with very few cases reported.3, 4, 5 In this article, we present a case report of Spinal Tuberculosis at an uncommon site i.e Lumbosacral junction which was treated successfully along with relevant review of literature.
Case Report
A 42 year-old gentleman presented with the chief complaint of pain in his lower back region from the last 3 months which was gradual in onset, progressive dull aching pain, bilaterally radiating to both lower limbs which was more on left side along with numbness. Patient had a history of low-grade fever and weight loss. There was no specific history of direct contact with TB patients. Patient is on Anti-tuberculosis medicine for the last 1 month.
On examination, the patient was calm, conscious, and well oriented to time, place, and person. His CVS, Pulmonary, and abdominal system were normal. There was no significant inspectory finding. On palpation, Localised tenderness was present over the lumbosacral region. His motor and sensory examination revealed no deficit in the upper limbs. However, in the lower limbs, plantar flexion at the ankle had a power of 4/5 MRC grading. Motor Power at Hip and Knee were normal. Sensory examination revealed impaired sensation to touch in the L5–S1 distribution in both lower limbs. Straight leg raise was 40 degrees on the left side. Knee reflex and ankle jerk were normally elicitable. Superficial abdominal reflexes were normally present. Plantar reflexes were absent on both lower limbs.
Investigations: Hematology reports showed 9 g/dl hemoglobin, elevated erythrocyte sedimentation rate (55 mm/1 h), and C-Reactive protein (20 mg/l). Other parameters were within normal range.
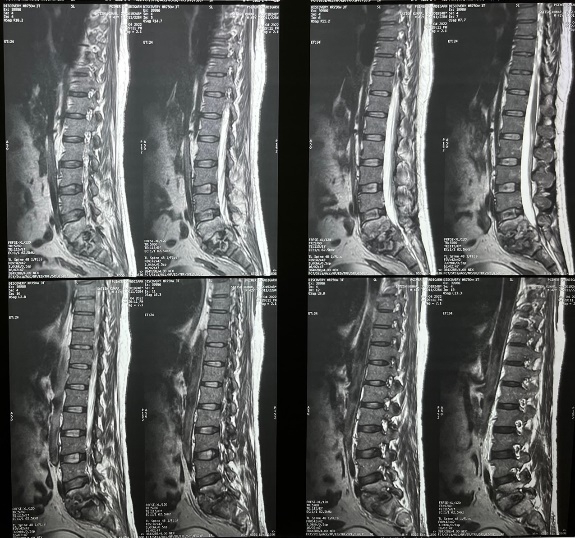
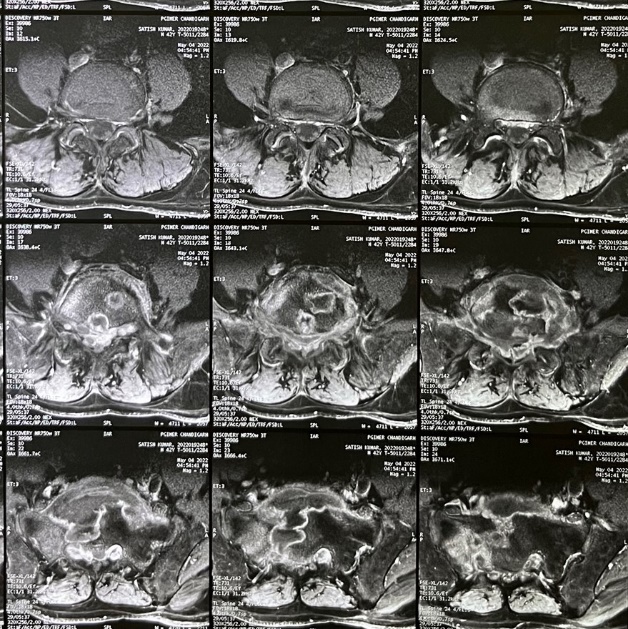
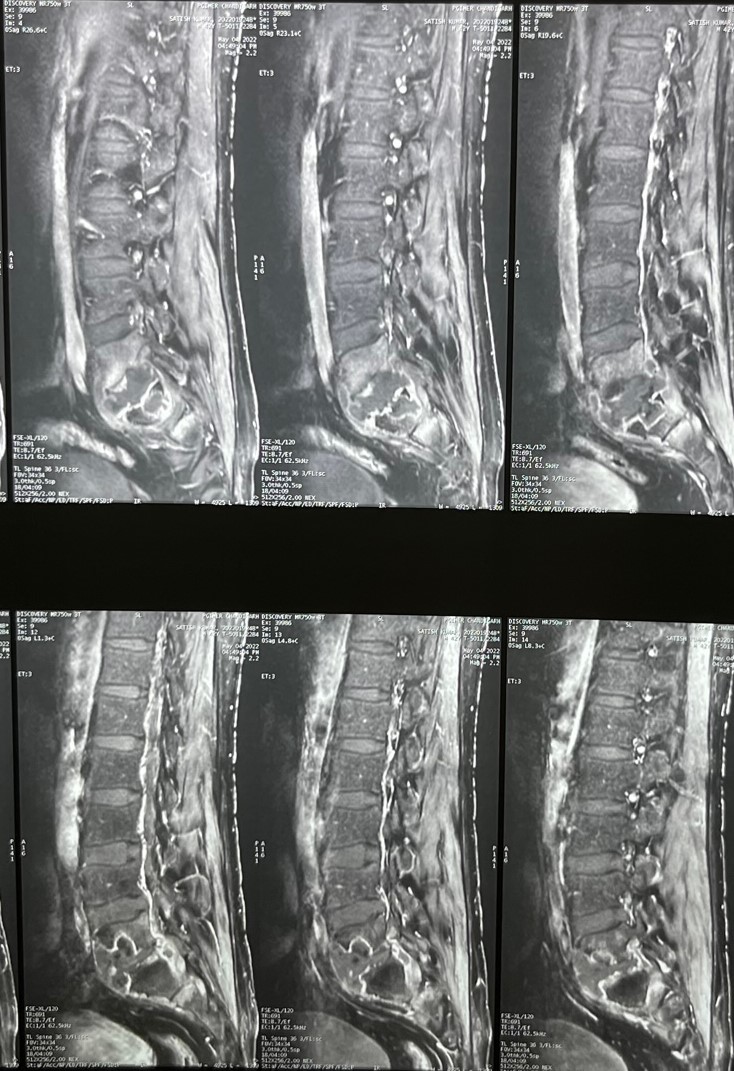
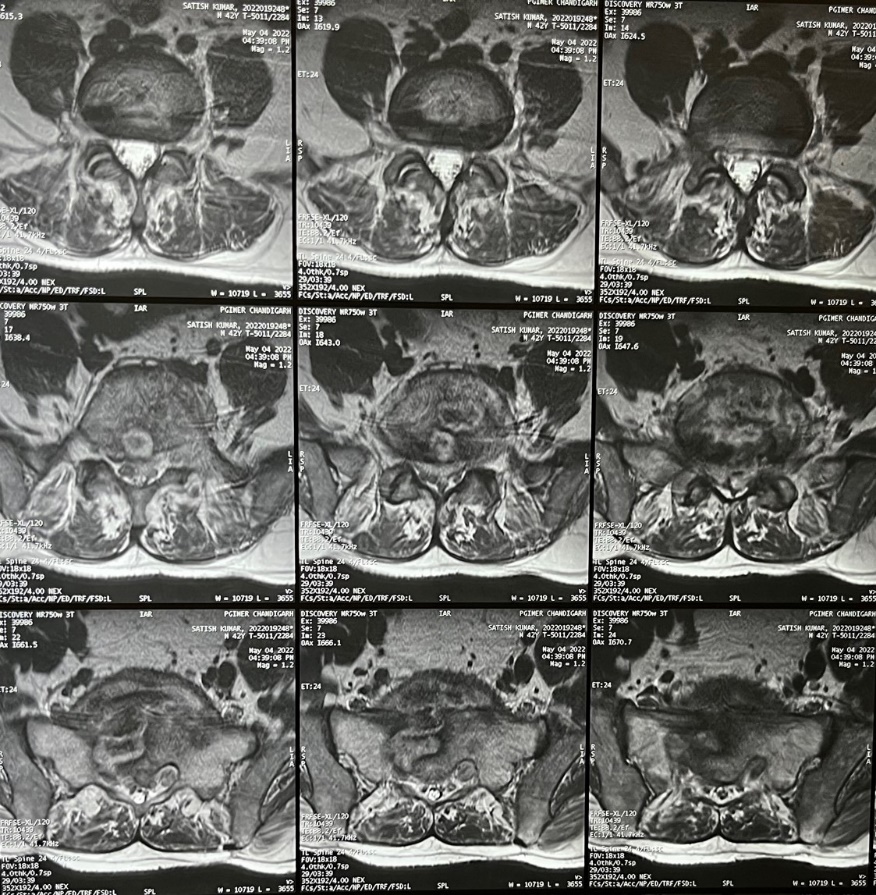
Plain Radiograph of the lumbosacral spine anteroposterior and lateral views showed reduced disc space between L5 and S1 with irregular margins (Figure 1). MRI of lumbosacral region T1-weighted, T2-weighted, and Short Tau Inversion Recovery (STIR), axial and sagittal images showed erosion and signal alteration in the L5 and S1 Vertebrae, altered signal intensity involving L5–S1 disc, and thecal sac compression (Figure 2, Figure 3, Figure 4, Figure 5).
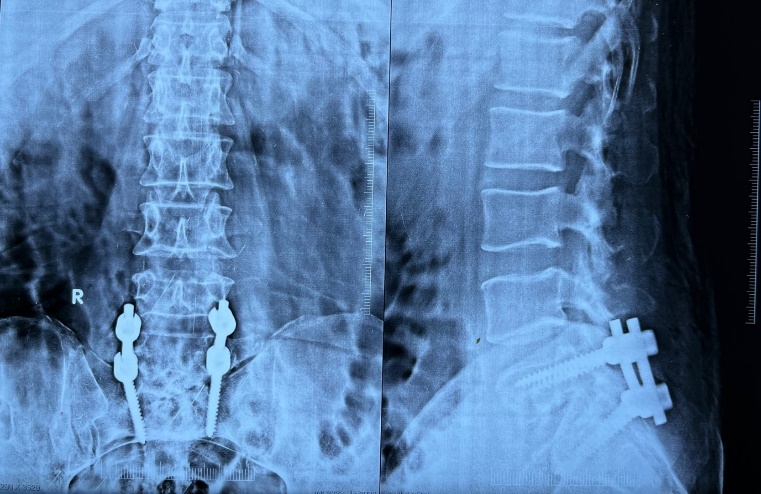
Treatment: The patient underwent posterior decompression and pedicle screw fixation at L5 and S1.(Figure 6) Granulation tissue which was present around the sac was removed and abscess was evacuated from the paradiscal region by cutting down the PLL. Bone graft was taken from the posterior iliac crest and L5-S1 transverse process fusion was done. Samples were taken and sent for Histopathology, CBNaat and for AFB culture. CBNaat and culture were positive for Mycobacterium Tuberculosis. Histopathological report showed granulomas with epithelioid cells and Langhans giant cells suggestive of tuberculosis. On follow-up, there was significant improvement and the patient was completely pain free.
Discussion
Tuberculosis has been around mankind for a very long time. Percival Pott first described tuberculosis of the spinal column in 1779, but till date, there are no acknowledged and clear-cut treatment guidelines available. Lumbosacral tuberculosis clinically presents with low back pain with or without neurological compromise.6, 7 This different behaviour of lumbosacral tuberculosis in comparison to other sites of the spine is due to the capacious spinal canal and floating nerve roots (relatively tolerant to compression by an abscess or by granulation tissue.8, 9 Diagnosis of spinal tuberculosis is made clinically, microbiologically and radiologically. Microbiological confirmation requires the demonstration of acid-fast bacilli on microscopy or culture of material obtained following a biopsy of the lesion.10 Polymerase chain reaction is a very effective method for bacteriological diagnosis of tuberculosis as it can detect as few as 10–50 tubercle bacilli.11 Radiological investigation comprised of plain radiographs, computed tomographic scan, and MRI. Disc space narrowing, irregular margins, abnormal paravertebral masses, and abnormal calcifications in the soft tissue are the usual findings on plain radiograph.12 CT helps in delineating the encroachment of the spinal canal by posterior extension of inflammatory tissue, bone, or disk material.13 MRI is the investigation of as it shows better details of the pathology and demonstrates spinal canal compromise.14 Once the diagnosis of skeletal tuberculosis is established, conservative management with an adequate course of antituberculosis can result in a good outcome.15, 16 Certain conditions such as compression of neural structures or persistent pain and/or instability demand surgical intervention under the cover of antitubercular chemotherapy are recommended.8 Potential benefits of surgery were less kyphosis, immediate relief of compressed neural tissue, quicker relief of pain, higher percentage of bony fusion, quicker bony fusion, less relapse, earlier return to previous activities, and less bone loss.17 Various surgical approaches are present such as anterior fusion, posterior fusion or combined approach. However, the approach used depends upon the symptoms and radiological findings.
Conclusion
Spinal Tuberculosis at lumbosacral junction is not only uncommon region wise but also behaves uncommonly with pain and minimal neurological deficits. Antitubercular therapy with surgical intervention is the mainstay treatment with added advantages of surgery such as thorough debridment and stabilization resulting in quicker pain relief and neurological recovery.