Introduction
The posterior shoulder dislocation is very uncommon scenario with incidence ranging from 3% - 5% of all different types shoulder dislocations.1 About 1 in 100 cases of shoulder dislocations involves a fracture of proximal humerus.2 Neer et al. reported 9 cases of the 15,000 shoulder injury cases have posterior fracture dislocations.3
Based on the mechanism of posterior shoulder fracture dislocations involves axial loading of flexed, adducted and internal rotated arm.4 A Reverse Hill-sachs lesion is seen in Posterior shoulder dislocation leading to an impaction fracture over the antero-medial surface of the humeral head. These cases can be complicated by a proximal humerus fracture and locking in the posterior dislocated position in some cases.5 Reverse Bankart lesion can also be present in posterior shoulder dislocations denoting avulsion of posterior capsular periosteum associated with detachment of postero-inferior labrum leading to laxity of the inferior glenohumeral ligament especially the posterior band.
Posterior locked fracture-dislocation of the shoulder (PLFDS) can be easily missed in up to 79% of cases as per some reports due to improper radiological investigations performed in the initial presentation.6 Locked internally rotated shoulder may be identified clinically with physical examination where lateral and forward abduction as well as external rotation are completely impossible. However, accuracy is compromised in physical examination due to the extreme pain associated with minimal movements.
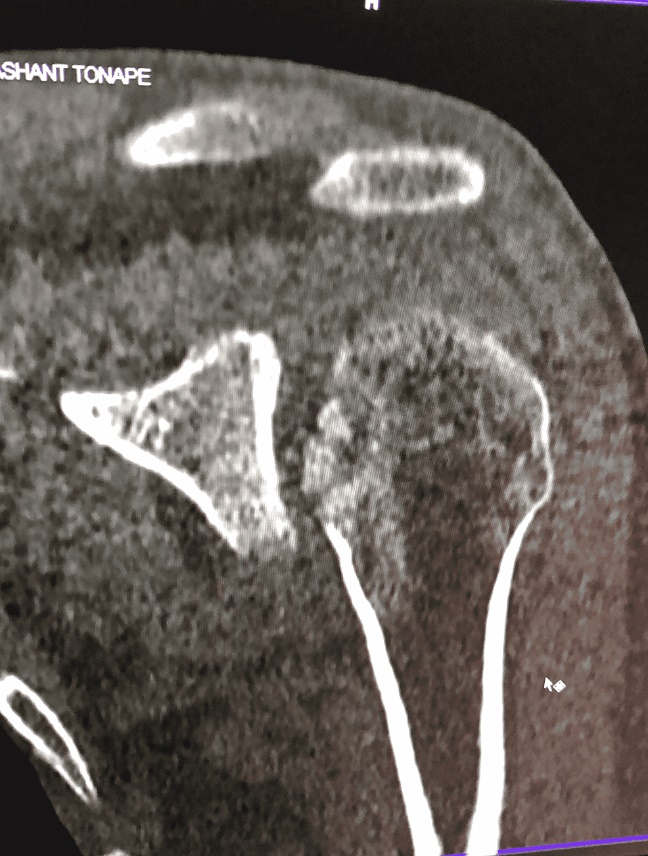
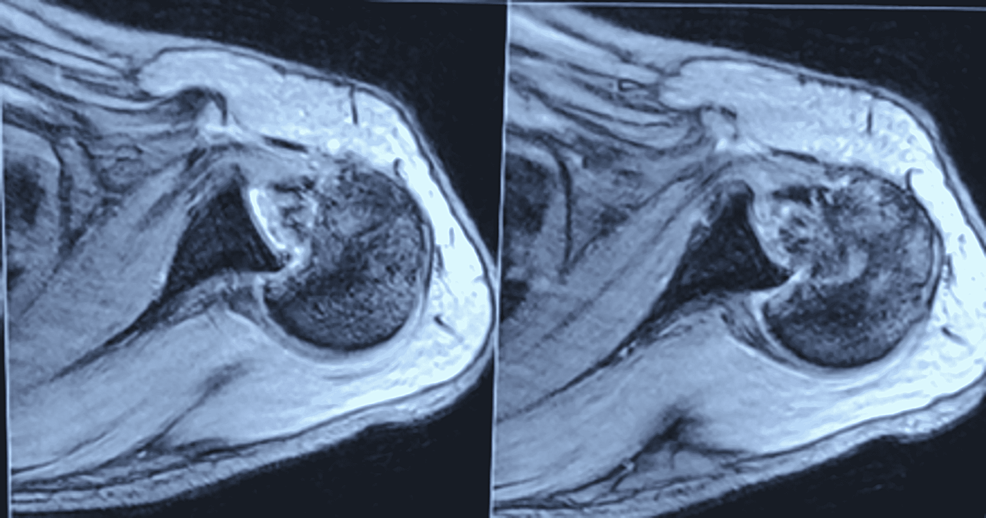
Posterior dislocation of gleno-humeral joint can be suspected with few x-ray signs. A conventional shoulder true anterior posterior view demonstrates an over imposing half-moon appearance due to the intersection of the head and glenoid; Secondly, lightbulb sign in posterior shoulder dislocation is seen due to the internal rotation of humeral head in AP View.7 Perhaps the most characteristic radiologic sign of PLFDS is the trough line sign where a dense vertical line in medial humeral head is seen due to impaction of humeral head.8 Nevertheless three trauma radiographic views are required for reliable diagnosis. If posterior locked fracture dislocation of shoulder is suspected, to assess the fracture anatomy and execute preoperative planning a CT scan is usually done. Articular surface involvement of humerus is assessed particularly with 3D reconstruction, Axial and coronal cuts. MRI may useful to rule out soft tissue and ligament injuries.
Fracture dis-impaction, transfer of lesser tubercle, defect filling with bone substitutes or allografts and reconstruction using k wires and plates are the treatment options in case of shoulder posterior dislocation associated with reverse Hillsachs lesion. The operating surgeon uses these options based on the amount of comminution and impaction.9 Various surgical options are closed reduction and pinning or, open reduction and internal fixation or, replacement arthroplasty.
The closed or open reduction and fixation of these fracture dislocations has become the preferred method of treatment, considering the lower costs and complications involved. The main aim is to maintain the integrity, anatomy and the vitality of the humeral head along with postoperative shoulder range of movements.10 In the choice of open reduction and internal fixation, approach and reconstruction of anatomy varies from surgeon to surgeon.
McLaughlin described a technique for the correction of PLFDS with reverse Hill Sachs lesion by subscapularis tendon transfer into the lesion and filling the defect was Hawkins et al. described the modification of McLaughlin procedure, in which both the tendon of Subscapularis along with Lesser tuberosity bone chunk were displaced and transferred into the Reverse Hill-Sachs lesion for stabilization.11, 12 The modified McLaughlin procedure is aimed to achieve a stable Glenohumeral joint as well as early and full functional recovery in cases of an acute posterior locked fracture-dislocation of the shoulder.13
Case Presentation
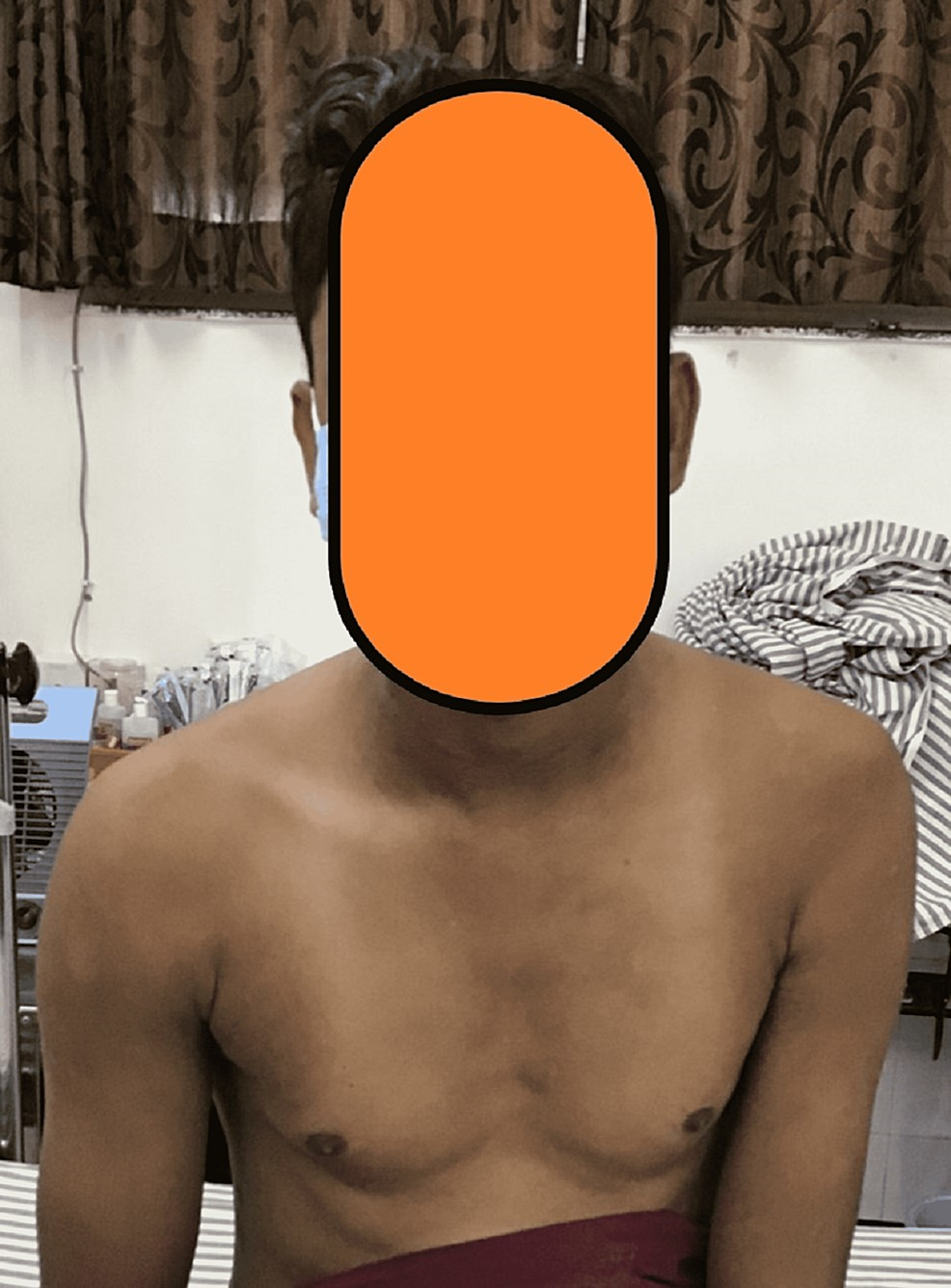
A 29-year-old man sustained a traumatic injury of left Shoulder due to road traffic accident 30 days ago. Patient presented with a wasting of musculature in arm and shoulder regions. Its Range of movements was minimal and painfully restricted. Radiographs and CT scan of left shoulder demonstrate PLFDS with a reverse Hill-Sachs lesion and reverse bony Bankart Lesion. Consents for publication were obtained and preoperative counselling was done. The patient underwent for a modified Mc Laughlin procedure.(Figure 1)
Figure 1
Pre-operative clinical picture showing wasting of the deltoid and other shoulder muscles due to disuse atrophy
Patient positioned in beach chair position and a small sandbag placed under scapula medial border to proud the affected side forward while allowing arm to have complete range of movements. Painting, draping and marking of the surgical site were done. A deltopectoral incision is made from distal to edge of clavicle and lateral to coracoid process. After incising the superficial fascia, the cephalic vein is identified and retracted medially. Delto-pectoral interval is extended down to open the clavipectoral fascia. After exposure, in view of fraying of long head of biceps tendon, a tenotomy and tenodesis were done.(Figure 5)
Figure 5
Modified Mc Laughlin surgical procedureA): Surgical planning to open the shoulder joint through Deltopectoral incision; B): Avulsion fracture of Lesser Tuberosity with Subscapularis insertion; C): A double loaded suture anchor placed into the bed of Reverse Hillsachs lesion; D): Final fixation with Screw and washer after the sutures of the anchor have been tied
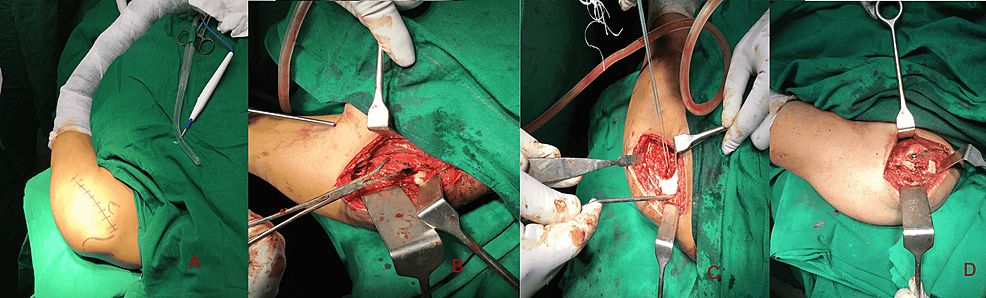
The lesser tuberosity as well as subscapularis tendon were dissected and reflected, held with a towel clip through fracture to expose the bony comminution beneath the lesser tuberosity of the humeral head. The tendon of subscapularis is released superiorly through the rotator interval. Minor bone fragments along with fracture hematomas are excised, because they cannot provide stability and reconstruction is difficult. Smaller impacted fractured bone pieces with articular surface is elevated up with a bone punch.
Gelpi’s Retractor and hand retractors were used in exposing the humeral defect. A needled double loaded suture anchor is impacted in the defect of humeral head due to the Reverse Hill-Sachs lesion after debridement. The medial suture limbs were passed further medial to lesser tuberosity fragment and through the substance of subscapularis tendon about 5-10 mm from its insertion. Two small drill holes were made through greater tuberosity with 2 mm k wire to enable the passage of two opposite sutures limbs through these drill holes to hold the fixation, later when sutures were tied.(Figure 6)
Transfer of subscapularis muscle along with lesser tuberosity into the reverse Hill-sachs lesion impression fracture done and a provisional fixation done with Kirschner wire passed through substance of lesser tuberosity and Reverse Hill-Sachs defect. Then, the sutures are tied down, snugly pulling into the reverse Hill-Sachs defect along with subscapularis tendon insertion and lesser tuberosity.
Figure 6
Schematic diagram of the Modified Mc Laughlin procedure with a Suture anchor and Cannulated screw
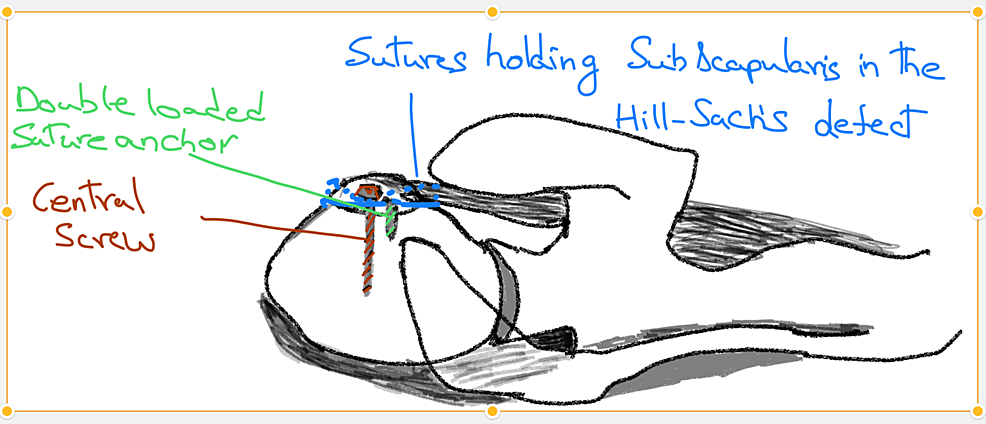
Another guide wire was passed through the fragments besides the Kirschner wire. A measured partially threaded, cannulated screw with mini washer is placed over the guide wire to achieve compression of the fragment of lesser tuberosity onto the humeral defect. The sutures were tied over the Subscapularis and Greater tuberosity, allowing enhanced fixation of the avulsed bony fragment. Internal and external rotation along with range of movements visualized. Gleno humeral joint reduction and screw placement confirmed by intra operative fluoroscopy.
An interrupted non absorbable suture was used for rotator interval closure. Subcutaneous tissue and skin were closed in layers over Romovac drain. Post op radiographs done to confirm fracture reduction and relocation of glenohumeral joint.
Post op physiotherapy protocol
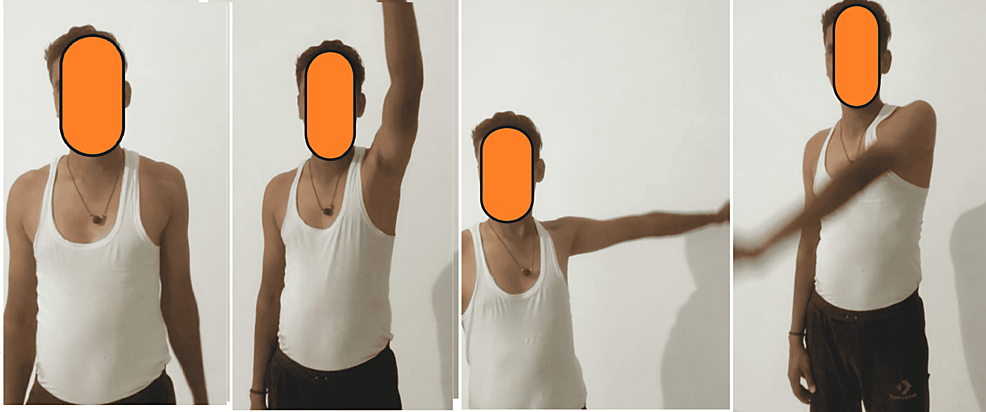
Postoperatively, the patient’s arm was placed in sling pouch for 6 weeks with passive pendulum exercises initiated after 3 days postop. At 4 weeks postoperatively, the arm sling pouch is discontinued and active range of motion was started. 2 months post op radiographs showed good glenohumeral reduction with fracture healing. Patient achieved complete range of movements with Constant-Murley Score of 100 out of 100 points by 3 months.(Figure 7)
Discussion
The conventional radiographic signs used to suspect posterior dislocation of the glenohumeral joint, such as the half-moon appearance and lightbulb sign, may be absent in cases of posterior locked fracture-dislocation (PLFDS) due to associated complex fractures.7, 8 Instead, the trough line sign, characterized by a dense vertical line in the medial humeral head, becomes a more characteristic radiologic sign.7 This highlights the importance of utilizing multiple trauma radiographic views and, if necessary, CT scans with 3D reconstruction and MRI to assess fracture anatomy and rule out soft tissue and ligament injuries.
When addressing shoulder posterior dislocations associated with reverse Hill-Sachs lesions, treatment options include fracture dis-impaction, transfer of the lesser tubercle, defect filling with bone substitutes or allografts, and reconstruction using K-wires and plates. The choice of surgical technique depends on factors such as the extent of comminution and impaction.9 Closed or open reduction and fixation have become the preferred methods, considering their lower costs and complications, with the aim of preserving the integrity, anatomy, and vitality of the humeral head and achieving postoperative shoulder range of motion.
The closed or open reduction and fixation of these fracture dislocations has become the preferred method of treatment, considering the lower costs and complications involved. The main aim is to maintain the integrity, anatomy and the vitality of the humeral head along with postoperative shoulder range of movements.10 In the choice of open reduction and internal fixation, approach and reconstruction of anatomy varies from surgeon to surgeon.
The McLaughlin procedure, initially described by McLaughlin and later modified by Hawkins et al., involves subscapularis tendon transfer into the reverse Hill-Sachs lesion and filling the defect.11, 12 The modification includes displacing both the subscapularis tendon and a chunk of the lesser tuberosity into the lesion for stabilization. This technique aims to achieve a stable glenohumeral joint and early and full functional recovery in cases of acute PLFDS.13
Previous studies have reported excellent outcomes in 25% to 45% of cases following a modified McLaughlin procedure for posterior locked fracture-dislocation. However, it is important to emphasize that physiotherapy plays a crucial role in the early rehabilitation of patients after shoulder surgery, contributing to their overall recovery and functional outcomes.14
Conclusion
The diagnosis and management of PLFDS with a reverse Hill-Sachs lesion poses specific challenges. The modified McLaughlin procedure, along with individualized treatment plans and postoperative physiotherapy, plays a crucial role in achieving a stable glenohumeral joint, restoring range of motion, and facilitating the patient's functional recovery.