Introduction
The primary osteoarthritis of the lumbar spine (OA lumbar spine) is age-related or degenerative arthritis of lumbar intervertebral joints (IV joints). It is found in both sexes, all over the world, and has existed since ages. In it, pain develops in the lower part of the back without any evident cause (hence the title primary). This occurs on movement of the back and subsides on rest. The disease progresses slowly, it's full clinical and radiological signs develop later.1 Most sufferers are past middle age (> 45 years) with a range of 18 to 60 years. The lifetime prevalence of back pain is 60- 80% and that of sciatica is 2-4%.2 As per the literature, its etiology and pathogenesis are not known.1 The basic lesion described is degeneration (weakening) of the disc and articular cartilage which progress with age and is aggravated by obesity, diabetes, and heredity.3 O A spine occurs more in manual workers particularly those who are in occupations involving heavy lifting and twisting of the back. Surgical and nonsurgical approaches are used for treatment. Emphasize exercise for its benefits, return to work, and manual activity, rather than bed rest.4 Use heat-assisted devices like lumbar belts and crutches to strengthen paraspinal muscles. Consider medication and injections of corticosteroids and anesthetics are the non-surgical method of treatment while Fusion (Arthrodesis) of affected segments and discectomy (Mini endoscopic Discectomy) are surgical methods of treatment.5
By the way, there is no cure for this disease. The treatment is based on pain management and mobility restriction. All the patients are initially treated with one or more non-surgical options which work for some time.
Surgery is advised on the failure of these regimens. Surgery has its disadvantages. Micro endoscopic discectomy (MED) done for prolapsed disc fails to relieve pain in 10% of operated patients and in those who got relief, it is not life-long. The commonest complication of a fusion operation done for O A, years later is either a return of back pain or a new symptom.6 O A spine usually increases year by year. In many cases, disabilities are bearable while in others increasing pain, stiffness, or deformity makes life miserable. The available literature lacks precise knowledge of the cause, pathogenesis, and treatment of this disease, similar to the case of primary osteoarthritis of the knee.7 This article aims to establish the same and assess the treatment results by a randomized controlled trial.
As per my hypothesis, this disease is a degeneration of all I.V. joints between the T12 to S1 vertebrae. The cause is a deficient full extension (DFE), pathogenesis capsular contraction in the front part of capsules, and treatment of their passive and active extension. The first two facts (cause and pathogenesis) are evidenced by a lateral skiagram which shows loss or reversal of lordosis in front and loss of Posterior concavity behind. Kyphosis is a late manifestation.
These changes come along the capsular contraction in front. On goniometry, the normal range of movement (ROM) of the lumbar spine (0° - 25°) is reduced. Here 0° indicates a neutral position and 25° backward bending. Details of these curvatures have been given in the discussion section. In essence, the cause is prolonged forward bending (done unknowingly for months or years); pathogenesis is the harm production (in the form of capsule contraction in the front part of I.V. joints) and treatment bending through passive and active extension of the spine. The treatment does not involve any surgical procedure, administration of a drug, application of physiotherapy, or use of any device.8
As per the theory, predisposing factors of the disease are:
Materials and Methods
Clinical Trial registration: ClinicalTrial.gov No. NCT 05693415.
Subjects
A total of 157 patients were taken into account for the investigation, of which 100 were in G1 and 57 in G2. Ages 30-90, back/leg discomfort, limited morning stiffness, and a lack of a history of injury, illness, or inflammation were used as inclusion criteria for the study, whereas exclusion criteria included neck pain, frozen shoulder, central obesity, acute lumbago, and X-rays of the spine that showed no symptoms of O A.
The trial was based on "Pragmatic Cluster Controlled Randomised Trial9 also known as a cluster randomized trial (CRT) or group randomized trial. In this variety, pre-existing groups called clusters of individuals were randomly allocated to treatment arms. My patients who consulted me were of two types. The type I wanted to avoid surgery had tried other non-surgical options e.g. drugs, physiotherapy, etc., and did not want them anymore. In this situation, it was not possible to give them any other treatment except the CCT. So those were included in the G1 and allocated to treatment. The type II patients were already using some options and living with disabilities but were not convinced to receive CCT so those were included in G2 and allocated 'no treatment.'
Procedure
The study setting consisted of my clinic, one charitable hospital, free weekly health camps, and clinics of two co-investigators. The study period was from 1st January 2021 to 30th June 2022. Informed consent was sought from all patients. The procedure consisted of 1. Baseline data recording 2. Treatment 3. Data collection and monitoring.
Baseline data recording
It consisted of recording name, age, sex, profession, predisposing factors (details given in introduction section), complaints with duration, deformity back, history of comorbidities (diabetes and obesity), side of the affected leg, straight leg raising test (SLR), detection - wasting and numbness and elicitation of reflexes.
Calculation of all three outcome measures
WOMAC5: Osteoarthritis score (0-96, 96 means worst) on the 5-point Likert-type scale.
ODI6 version 2: Oswestry Low Back Pain Disability Questionnaire, 0-100% (0% = no problem, 100% worst) measured in ten domains, each 0-5 score.
Formula - Disability % = 100/50 x score count.
VAS7: Visual Analog Vertical Scale 20cm for measuring pain (0-100, 100 means no pain).
Treatment
The treatment was intended to correct the front part capsule contracture in lumbar joints by intermittent, sustained passive extension and active extension of the back - Contracture Correction Therapy (CCT). It consisted of the following parts:
Immobilization spine when pain was severe
The passive extension (Postures 1-6,) and active extension (Postures 7 - 11) of back
Three therapeutic rituals - viz. Sleep in prone and rise in prone (Posture 12 - 14), sky watch (Posture 15, Figure 1), and drinking water with extended neck (Posture 16, Figure 1).
Advice to avoid stooping. For details, please see Figure 1.
Figure 1
Summarization of different posture to treat where: Posture 1 Relaxed body lying in prone (Makar asana in yoga science) Posture 2 Relaxed body in prone with hands under forehead, Posture 3 Relaxed body in prone with hands under chin, Posture 4 Relaxed body in prone with head raised on palms, Posture 5 Relaxed body in prone with knees flexed, Posture 6 Relaxed body in prone with legs pulled by hands, Posture 7 Raised head and chest, hands near forehead, Posture 8 Raised body, hands under shoulders., Posture 9 Raised head and chest, forearms kept across back, Posture 10 Raise both legs, with fists under groin, Posture 11 Raise both legs and trunk, fists under groin, Posture 12 Raise head and trunk during rising in bed, Posture 13 Raise head and trunk and buttock - hand knee position, Posture 14 Sitting between heels, Posture 15 watch in standing with forearms across back, Posture 16 Drinking water with extended neck
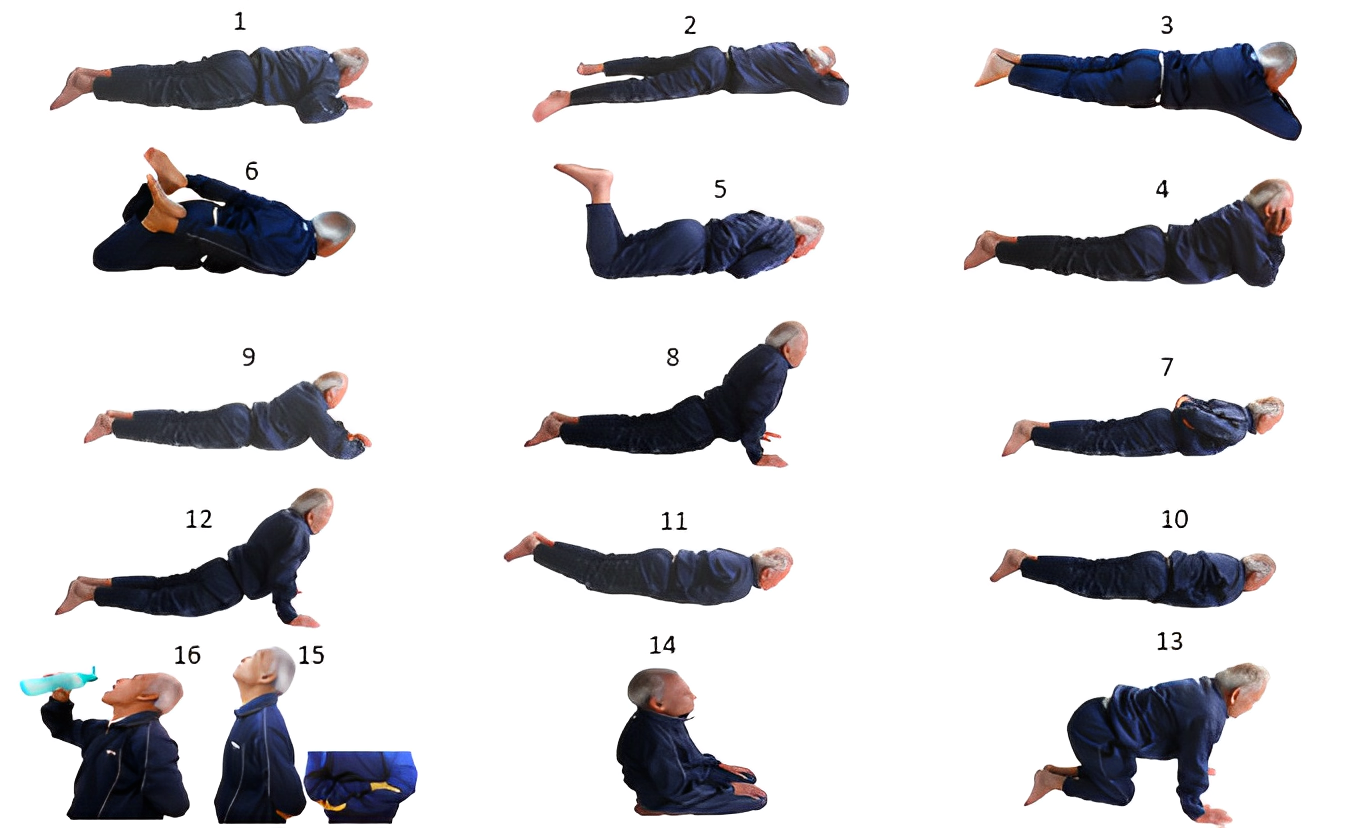
Table 1
The treatment modalities applied in trial
Table 2
Showing harmful and beneficial factors in OA spine
Outcome measures
To assess the results, the primary outcome measures consisted of WOMAC, and the secondary consisted of ODI and VAS at the beginning and end of the follow-up. These measures were also used to compare the results between G1 and G2.
Statistical analysis
The statistical analysis was performed by using IBM SPSS-22. Paired t-test/Wilcoxon signed-rank test was used to compare the clinical scores of WOMAC, ODI, and VAS at baseline and endpoint while an independent t-test/Manwhitne test for comparing outcome data between G1 and G2. The value of P<0.00 was considered statistically significant.
Results
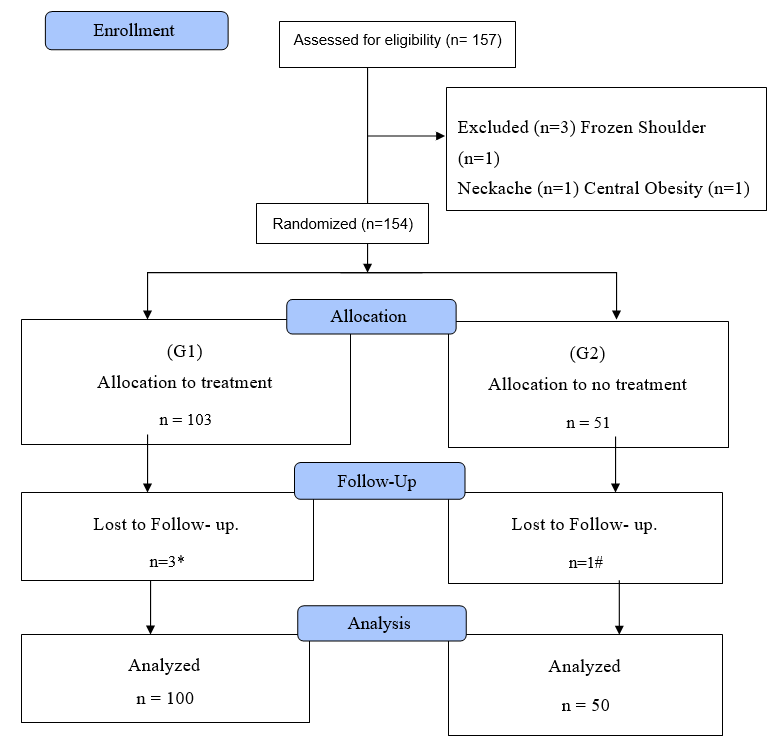
A consort (CON = consolidated, S = standards, O = of, R = reporting, T = trials) chart has been presented for the trial - Figure 2.
Figure 2
Consort chart
*Died of Stroke – (n=1), * Got Corona – (n=1), *Untraceable – (n=1), #Underwent surgery –(n=1)
The baseline characteristics of the subjects have been shown in Table 4.
Table 3
Important characteristics of subjects
Among legs affection L-20%, R-10% and both 5% in G1, while these figures were 24%, 8% and 4% respectively in G2. Diabetes type 2 in 17%, Obesity in 5%, positive SLR test 16% in G1 and 8%, 2% and 4% respectively in G2. The results of all three outcome measures at all different periods have been shown in Table 5.
Table 4
Details of all outcome measures at different periods in both groups
As per the Table 5 average WOMAC score fell from 54.29 to 0.00 and ODI from 51.82 to 0.00 in G1. The similar fall in G2 was 56.40 to 4.08 and 65.10 to 6.00 only from baseline to endpoint. VAS score rose from 37 to 100 in G1 and 34.4 to 81 only in G2. The fall in WOMAC and ODI and the rise in VAS indicate improvement by treatment. The treatment was much more effective in G1, while less in G2 (Table 5). This was according to the Independent t-test.
Table 5
Comparison of average clinical scores in both groups at initial and end points
|
S. No. |
Outcome Measure |
G1 |
G2 |
||||
|
0 week |
24 weeks |
P value |
0 week |
24 weeks |
P value |
||
|
1. |
WOMAC |
54.29 |
0.00 |
0.00 |
56.40 |
4.08 |
0.00 |
|
2. |
ODI |
51.8 |
1.8 |
0.00 |
65.10 |
6.0 |
0.00 |
|
3. |
VAS |
37.56 |
100 |
0.00 |
34.40 |
81.00 |
0.00 |
Besides the statistical data, clinical improvement in G1 was also superior in G2 (Table 6).
Table 6
Treatment result analysis according to clinical relief
Discussion
The hypothesis was regarding three parts of OA spine viz cause, pathogenesis, and treatment. Out of these, treatment was proved through experiments while the other two by deducing from its results. When the passive extension and active extension as treatment were found to be effective, the related cause and pathogenesis were presumed to be proven.
The vertebral column is a bony structure situated in the Posterior part of the body between the head and redundant tail. Divided into four parts - cervical, thoracic, lumbar, and sacrococcygeal is meant to give shape and mobility to the trunk. The lumbar part is situated in the back of the abdomen, concave behind, and convex in front. It is composed of five vertebral bodies (L1-L5), and six I.V. joints between T12 – S1. The joints give movements to the trunk - flexion, extension, lateral flexion, and backward turning. Each joint is composed of two bones, a capsule, two articular cartilages, a disc, a synovial membrane, and synovial fluid.
Synovial fluid is produced by the synovial membrane, transported by mutual movements between the constituting bones, and is the sole supply of oxygen and nutrition to discs and cartilages. The disturbance to its supply gives rise to asphyxia and starvation leading to their necrosis. The discs soften and herniate out by body weight upon them. Because cartilage is a neural, cartilage damage in joints is not accompanied by pain.10 The same thing applies to disc damage. Articular (Hyaline cartilage) and disc (Fibrocartilage) both do not possess blood vessels, lymphatics, and nerves.11 Disc damage was supposed to be the cause of prolapsed disc syndrome and OA spine. These anatomical facts show that the disc and articular cartilage cannot be the seat of this disease as they are insensitive to pain. The pain in this condition develops only on joint movement which indicates that responsible structure must be capable of undergoing momentary change. This criterion is fulfilled only by the joint capsule.
Anybody structure or tissue, due to any cause when it does not perform its function, loses its functional capacity and gets lost.7 The uterus after menopause cannot conceive, knee in a plaster cast for some time cannot flex, exhibiting DFF and shortening in the anterior part of its capsule. An immobilized elbow in a semi-flexed position neither can fully flex nor extend soon after plaster removal.
In the lumbar spine, long-standing DFE (i.e., extension up to 25o) reduces the lengthening capacity of anterior parts of I.V. joints capsules and hence, that part of the capsule loses elasticity (loss of elastic fibers), contracts (fibrosis), and hardens (calcification). Sudden straightening of the trunk (climbing stairs or lifting weight) from a stooped position causes stretch on the contracted capsule and gives pain. The capsule contracture is the primary lesion. Later, secondary damage occurs in discs (softening, flattening, and herniation), cartilage (necrosis), and bones (subchondral sclerosis). Any functional or structural change in the joint leads to its osteoarthritis often many years later.1
The improved outcome measures (Table 5) and clinical results (Table 6) indicate that the unknown factors (cause, pathogenesis, and treatment) are discovered, and the hypothesis is proven (Table 7).
Table 7
Important aspects of the obtained results
|
S. No. |
Result Summary |
Interpretation |
Significance |
Whether proves hypothesis |
|
1. |
WOMAC fell 54.29 to 0.00 |
Decreased score signifies measurable improvement |
Quantitative proof of cure12 |
Yes |
|
2. |
ODI fell 51.8 to 1.0 |
Decreased score signifies measurable improvement |
Quantitative proof of cure13 |
Yes |
|
3. |
VAS rose 37.56 to 100.00 |
Increased score signifies measurable improvement |
Quantitative proof of cure14 |
Yes |
|
4. |
Relief in symptoms (Table 7) A. G1 1. Full Relief 96% 2. Partial Relief 2% 3. No Relief 1% 4. Complications 1% |
CCT cured a large percentage of patience |
Proof that CCT is a specific treatment |
Yes |
|
B. G2 1. Full Relief 4% 2. Partial Relief 40% 3. No Relief 6% 4. Complications 50% |
Non-CCT cure was a much less percentage of patients |
Proof that Non-CCT was almost ineffective |
Yes |
To the best of my knowledge, this study is the first of its kind. Here the OA lumbar spine has been described to be present in three forms viz. low back pain, sciatica, and prolapsed disc syndrome while in literature all three have been described separately. Their cause is given to be unknown with suspicion on damage to the articular cartilage and discs. As both these structures are aneural, their association with pain is unlikely. As per my hypothesis, primary damage occurs to the capsule (responsible for pain) and then secondary to cartilage and disc.
As per Maheshwari15 low back pain is more common in surgeons, dentists, miners, and truck drivers. This fact coincides with this study where the highest incidence (46%) is of stooping as a predisposing factor (details in the Introduction section). The hypothesized treatment (CCT) looks superior to those described in the literature. There is a drawback in this therapy that the elongation in the contracture is short-lived which necessitates its frequent sessions. The steps of this therapy look like an imitation of physiotherapy and exercises which undermine their impression. Future research should be directed to obtain permanent/long-lasting correction of the contracture so that the CCT may not be a lifelong necessity. Another field of research will be to design a lifestyle that will prevent the disease automatically. At present, according to the literature, the cause and specific treatment of this disease are not known. The results of this study will remove this lacuna. The addition of these facts will enhance the knowledge of this disease and improve its treatment. By the results of this study, there can be vast changes in clinical practice. So far the disease is being treated by orthopedic and general surgeons, physiotherapists, and quacks by various surgical operations, medicines, and devices without an unfounded basis. Now the treatment shall be fixed and easy and would be carried out by orthopedic and general surgeons, and even by general medical practitioners.
Though the follow-up period in the study is 24 weeks only, the therapy is in practice since 2005 and continuing.
Conclusion
The study focused on the primary factor contributing to the difficulties in sitting, climbing, and walking caused by primary osteoarthritis of the lumbar spine. The person lacks his or her physical activity in the early stages. Typical medical care is ineffective and only temporary. For six months, 154 patients participated in a trial of a novel treatment. Based on obtained results, it can be concluded that Osteoarthritis of the lumbar spine results in protracted incomplete extension; etiology entails contracture formation; and therapy entails passive and active extension.
