Introduction
Named after Abraham Colles in 1814, distal radius fracture, also known as “Colles fracture,” is a common fractures found in day to day practice.1, 2 Among the many classification systems, the Fernandez classification, which is based on the mechanism of the fracture, has the highest inter-observer agreement.3 Treatment of this common fracture was conservative for a long time, even before the era of the discovery of the X-ray, but in the last few decades, the treatment of distal radius fractures has greatly shifted to the operative side. Apart from conservative management, many other treatment modalities are available, such as closed reduction followed by percutaneous pinning (CRPP) with K-wire, bridging and non-bridging external fixation (relying on the principle of “ligamentotaxis”), plate fixation and even intra-medullary nail (IMN).4, 5 Closed reduction of fractures and immobilization by plaster cast application or functional cast bracing for the treatment of distal radius fractures is still a common practice.6, 7 For distal radius fractures, closed reduction followed by percutaneous pinning (CRPP) with K-wire is frequently performed surgery nowadays, as it is less invasive and less demanding surgery.8 Though CRPP has improved in radiological outcomes, it does not help to improve the functional outcome compared to the very old-aged practice of conservative methods for treating distal radius fractures and both also have similar low complication rates.9 There are no consensus guidelines for choosing the optimal treatment modality for a particular distal radius fracture. According to AAOS, it is not only based on the physician, but also on mutual communication between the patient and other healthcare practitioners. It is also important to keep in mind that the procedure which is simpler, less invasive, and able to control the fracture variables should be opted for.10, 11 Therefore, in this era of operative intervention, this study aims to analyze the outcomes (radiological, clinical, and functional) of distal radius fractures managed conservatively (closed reduction and cast application) and with percutaneous pinning (K-wires) and to determine if there are any significant differences.
Materials and Methods
This study is an institutional-based prospective comparative study, comprised of 50 adult patients between 20 to 65 years of age with distal end radius fractures attending the Department of Orthopaedics, Medical College and Kolkata, India. Clearance from the institutional ethics committee and informed consent of the patient are taken. Routine blood investigations are done. Among them 25 patients were treated with closed reduction and plaster cast immobilization(CRPCI) and 25 patients were treated with closed reduction and percutaneous pinning (CRPP) with K-wire who fulfilled the study criteria, during the period January 2021 to June 2022, the study was conducted for 18 months. Criteria for inclusion were patients aged between 20-65 years, fractures less than 7 days old and Fernandez Type I fracture. Exclusion criteria were open fractures, other types of Fernandez fractures, associated life-threatening injuries, pathological fractures, osteochondral defect and a history of surgery due to fracture radius or fracture of surrounding bones.
Closed reduction and plaster cast immobilization (CRPCI)
The closed reduction was made under sedation or hematoma block or brachial plexus block. For reduction, Jones’ method of fracture reduction is used which involves applying traction, counter-traction was given by an assistant by holding the arm in a flexed elbow. First deformity is exaggerated then the distal fragment is volarly flexed and stabilizes the wrist in slight flexion and ulnar deviation. Reduced position is checked under fluoroscopy. After a good reduction i.e. within the acceptable criteria for distal radius reduction 6–8 layers of plaster of Paris cast were applied. Then plaster cast was applied and moulded to give three-point fixation and allowed to become hard rigid. Below elbow plaster cast was applied. Both anteroposterior, lateral wrist radiographs were taken to confirm the reduction and alignment. After the anesthetic effect was gone patients were allowed to actively move their fingers, elbow and shoulder joint. Patients were kept for five to six-week cast immobilization. The plaster cast was removed after 5-6 weeks after seeing radiographic healing of the fractures. Functional use of the hand is allowed after 8 to 10 weeks.
Closed reduction and percutaneous pinning (CRPP)
The operation was done under a brachial plexus block or general anaesthesia. A prophylactic antibiotic (1g of cefazolin) was injected intravenously after proper skin testing. After painting and draping, for reduction, Jones’ method of fracture reduction is used which involves applying traction and counter-traction that is given by an assistant by holding the arm in a flexed elbow. First deformity is exaggerated then the distal fragment is volarly flexed and stabilizes the wrist in slight flexion and ulnar deviation. Reduced position is checked under fluoroscopy. Maintaning the fractures in reduced position, correct starting point for k-wire placement are assured with fluoroscopy and then finally k-wire were placed under c-arm guidance. We use at least two to three k-wires to maintain the reduction in all planes. All k-wires are engaged both near and far cortex for good purchase in metaphyseal bone. Fracture stabilities are tested by doing movement of wrist joint under fluoroscopy. K-wire then bends and cuts them, leaving a small length outside the skin for easy removal later. We applied below elbow plaster of the Paris slab to further stabilizes the fracture.Post-operatively patients were allowed active finger movement immediately as per patient pain permit. Active and active-assisted range-of-motion exercises of fingers, elbow and shoulder are begun. The below elbow plaster of the Paris slab and pins are removed after the 5th to 6th weeks of post-operative period.
Table 1
Radiographic parameters of patients with distal radius fracture
Table 2
ROM of patients with distal radius fracture
Outcome measures and statistical analysis
Data received from the study was analyzed for radiographic outcome, range of motion of wrist joint and functional outcome by using the Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH). For pain we used Visual Analog Scale (VAS) at 1yr of follow up and results were analyzed by IBM SPSS Statistics software version 28.0.0.0.
Results
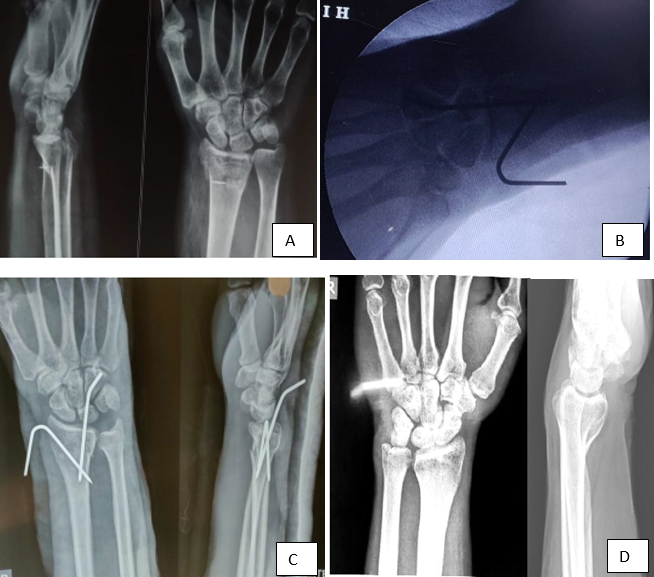
All fractures were united by 3 months when radiographs were taken on follow-up (Case 1-4). The age of patients in this series ranges from (20-65) years with a mean of 54yr and the maximum patients (72%) were in the (51-65) years age group. The majority of the patients were female (66%).8% of patients who underwent percutaneous pinning developed pin track infection. 'P' value for this association was 0.49 which is statistically insignificant. Radiographic parameters and range of motion (ROM) of wrist joint are shown in Table 1 and Table 2 respectively.
In our study functional assessment by DASH score shows a p-value of 0.90(>0.05) which is statistically insignificant i.e. there is no significant differences in functional outcome between patients treated with CRPCI and patients treated with CRPP at 1year follow-up. There is no significant difference in pain after 1year of follow-up as per VAS. The mean VAS score in CRPCI treated group is 2.24±1.28 and CRPP group is 2.20± 1.08( p-value 0.59).
Case 2
CRPCI-2 (Closed reduction and plaster cast immobilization) (Figure 2, Figure 3)
Case 3
CRPP-1(Closed reduction and percutaneous pinning with k-wire) (Figure 4, Figure 5)
Discussion
Distal radius fractures are one of the most common fractures found during day to day clinical practice. Although the most recent guidelines developed by the American Academy of Orthopaedic Surgeons (AAOS), Cochrane systematic review, both are inconclusive to determine the best treatment option for a distal radius fracture among the various surgical and nonsurgical treatments available.In this study, the mean age of patients is 54 and a maximum of patients (72%) in the (51-65) years age group with the majority of the patients being female 66%. Marcus Landgren et al. in their study show a mean age of 48 (20–65) years which also supported that age group.12 Kate W. Nellans et al., Chung et al., and Spilson et al. in their study supported female preponderance.13
This study shows radial inclination is less in the CRPCI group than in the CRPP-treated group, there is a statistically significant difference between the two groups of patients. The mean radial inclination in CRPCI treated group was 13.48 ± 2.00 and in CRPP treated group was 18.12 ± 1.23. The p-value was 0.017 (p value <0.05) which is statistically significant. Wong et al study shows the conservative group had significantly less radial inclination than the operative group (collective mean SD=1.40,P=0.001).The current study also matches this.14
The mean Radial Height in millimeter in CRPCI treated group was 3.04 ± 4.015 and CRPP treated group was 9.20 ± 2.55.The p-value was 0.026(p value <0.05) which is statistically significant. Rafael J. Diaz-Garcia et al and others, multiple comparison analysis shows, there are significant differences(more in operative group) in radial height between conservative group and all other treatment groups (p<0.001).15
The mean Ulnar Variance in millimeters in CRPCI treated group was .88± 1.45 and the CRPP treated group was -1.68± 1.145.The p-value was 0.021(p value <0.05) which is statistically significant. Ji-Hui Ju et al.,16, Aktekin et al.,17 and others shows the surgical group had significantly lower ulnar varience than the conservative group (collective mean SD =−0.82,P<0.001). All these studies support our study result.
Regarding the volar tilt, there are no statistically significant differences between the two groups of patients are noted. The volar tilt in CRPCI treated group was 0.68 ± 4.432 and CRPP treated group was 7.76 ± 4.024. The p-value was 0.138(p value>0.05) which is statistically insignificant. However multiple comparison studies shows, there are significant differences in volar tilt between the conservative group and all others surgical treatment groups (p<0.001).18
The study also shows, among the CRPCI group, no one is suffering from infection but 8% of patients of the CRPP group. The 'P' value for this association was 0.49 which is statistically insignificant. Kristina Lutz et al study shows a significant number of patients experienced complications like surgical site infection including pin track infection.19
In this study, there are no statistically significant differences in wrist dorsiflexion (p-value was 0.112), palmar flexion (p-value is 0.941), Pronation (value was 0.782), supination (p-value is 0.318), radial deviation (p-value was 0.881) and ulnar deviation (p-value was 0.826) (p value>0.05) between CRPCI and CRPP treated group. Wong et al.,14, Arora et al.,20, Lutz et al.,19 , and others show no significant difference in the range of wrist movement between the operative and nonoperative groups was noted (P=0.260). All these support our study.
DASH score shows a p-value 0.90 (>0.05) which is statistically insignificant i.e. there is no significant difference between patients treated with CRPCI and patients treated with CRPP for at 1year follow-up, which is similar to the above study. Chan et al. in their analysis of DASH scores comparison of the operative and non-operative groups showed little difference or no difference in DASH scores at 6 to 12 month follow-up.21 No significant difference in pain after 1year follow-up as per VAS score p-value 0.59(>0.05). The mean VAS score in the CRPCI group is 2.24±1.28 and the CRPP group is 2.20±1.08.No significant differences in functional assessments were found when comparing CRPCI and CRPP management of fractures distal radius. Small sample size, short follow-up period all are limitation of our study.
Conclusion
Distal radius fractures are one of the most common fractures found in day to day clinical practice. The treatment is controversial and still debated in the literature. This study shows though poor radiographic outcomes associated with conservative management than closed reduction and percutaneous pinning but there were no differences in functional outcomes.