Introduction
Proximal tibia extra-articular fractures are complex injuries that occur near the knee joint but do not involve the articular surface.1 Proximal tibia fractures can be due to a range of injuries and mechanisms and are associated with different severity. These types of fractures usually result from high-energy trauma. The tibia diaphysis is the most common site of fracture in the tibia and about 80% of these injuries are associated with fibular fractures.2, 3 There are various treatment modalities for operative management of these injuries - open reduction and internal fixation, external fixation and intramedullary nailing (IMN).4 The current treatment modality for surgical management of proximal tibia extra-articular fractures is intramedullary nailing. Intramedullary Nailing allows for Less soft tissue disruption, conservation of the periosteal blood supply, early mobilization and weight-bearing.5Traditionally, an infrapatellar approach has been used for this operation either by a transpatellar tendon split or by retracting the tendon medially or laterally. Proximal third extra-articular proximal tibia fractures can be difficult to treat through this approach as hyperflexion of the knee is required to gain an adequate entry point, which can lead to further displacement of the fracture because the quadriceps muscle forces the proximal fragment into extension, resulting in deformities of angulation and fragment displacement. Chronic postoperative knee pain is one of the most commonly reported complications of intra-medullary nailing (IMN) insertion with the incidence rate varying from 10-80%.6 Nowadays, the suprapatellar approach with the knee in a semi-extended position is gaining popularity due to its benefits, including easier fracture reduction, accurate nail entry point, a shorter operating time and lower radiation exposure.7 The semi-extended position helps in the fracture reduction of apex anterior deformity while avoiding the patellar tendon. This leads to lower levels of chronic knee pain after operative intervention, or even the absence of pain because the suprapatellar route does not injure the patellar tendon. Supra patellar approach is also proposed to be effective in reducing the incidence of postoperative knee pain and preventing a degenerative disorder of the knee joint. However, some studies showed that intra-articular injury may be a potential complication of this technique. With the suprapatellar approach becoming more recognized and utilized in the management of proximal tibia fractures, this study was performed to compare the functional and radiological outcome of the suprapatellar versus infrapatellar approach for proximal tibia extra-articular fractures using intramedullary nails.
Materials and Methods
This randomized controlled study was conducted over 24 months in the Department of Orthopaedics, Maharishi Markandeshwar Institute of Medical Sciences and Research (MMIMSR) Mullana-Ambala. The study aimed to compare the functional and radiological outcomes, between Suprapatellar and Infrapatellar intramedullary nailing techniques in the treatment of proximal tibia extra-articular fractures.
Patient Selection
A total of 40 patients with proximal tibia extra-articular fractures were included in the study. Patients were eligible if they met the following criteria:
Inclusion criteria
Patients with in age between 20 to 70 years with closed fractures of both bone leg, segmental fractures of tibia, all extra-articular fractures of tibia and Patients who are ready to give consent for study are included in the study.
Exclusion criteria
Patients with Paediatric fractures of tibia, Pathological fractures of tibia, Associated comorbidities like Uncontrolled diabetes or hypertension, deranged hepatic or renal functions, Intra articular extension fracture in knee and ankle, Stiff knee, Open/ Compound fractures, Pre-existing OA knee or/and previous knee injury and patient who are unwilling to give consent for the study are excluded from the study.
Randomization
Patients were randomly assigned to one of two groups using simple randomization with a random number generator:
Operative protocol anaesthesia:
Spinal Anaesthesia / General Anaesthesia Preparation: The limb was scrubbed with an aqueous iodine-based solution thoroughly from the thigh to the foot and draped with sterile sheets.
Surgical Procedure
All surgeries were performed by experienced orthopedic surgeons in the department of orthopedics, Maharishi Markandeshwar Institute of Medical Sciences and Research (MMIMSR) Mullana-Ambala using a standard intramedullary nailing system.
Approach
Infrapatellar approach: The skin incision give infrapatellar (Figure 1). The “ideal” entry point for insertion of a proximal tibia nail has been described as being 2 mm medial to the lateral proximal tibia spine on AP imaging and immediately adjacent and anterior to the articular margin of the medial proximal tibia plateau on lateral imaging.8
Suprapatellar approach: 1.5-cm to 2-cm longitudinal skin incision is made 1 cm above the base of the patella (Figure 2 ). The quadriceps tendon is exposed by blunt dissection and a longitudinal midline split is performed in the tendon.8
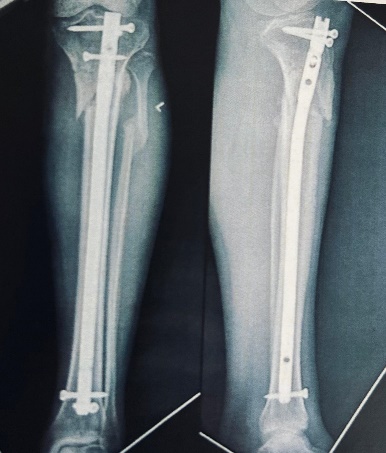
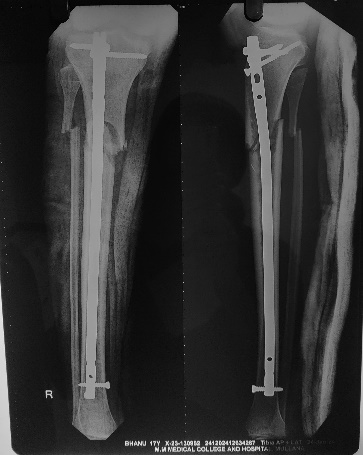
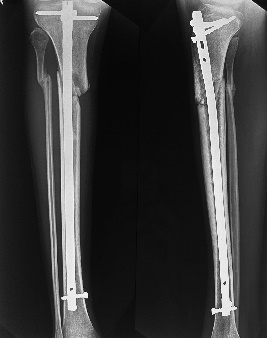
All patients received preoperative antibiotics and had closed reductions guided by images (Figure 3, Figure 6). Weight-bearing and mobilization were part of the standardized postoperative procedures for both groups. To guarantee adequate implant placement and fracture reduction, radiographs (Figure 4, Figure 7) were taken after surgery.
Outcome Measures
Functional Outcomes
Functional outcomes were assessed using the Lysholm Knee Score9 and the Lower Extremity Functional Scale (LEFS)10 at 1 month, 3 months and 6 months postoperatively:
A) Lysholm Knee Score: A knee-specific scoring system assessing stability, pain and function.
B) LEFS: A validated scale measuring lower extremity function in daily activities.
Pain Assessment
Pain levels were measured using the Visual Analog Scale11 (VAS) at 1, 3 and 6 months postoperatively. Patients rated their pain on a scale from 0 (no pain) to 10 (worst pain).
Radiological Outcomes
Radiological outcomes were assessed via standard anteroposterior (AP) and lateral radiographs to evaluate the following:
Statistical Analysis
Statistical analysis was performed using [software, e.g., SPSS or R]. Continuous variables, such as functional scores (Lysholm, LEFS), VAS scores and operative times, were compared using independent t-tests. Categorical data were analyzed using the Chi-square test. A p-value <0.05 was considered statistically significant.
Sample size calculation
Based on previous studies comparing functional outcomes between the two approaches, a sample size of 20 patients per group was calculated to provide 80% power to detect a difference in Lysholm Knee Scores at 3 months, with a significance level of p < 0.05.
Post-operative protocol
Immediate Post-Operative Care (Day 1 to Week 2)
All patients were provided with standardized post-operative pain management, which included the use of oral analgesics such as acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs).
Post operative x- ray (Figure 4, Figure 7)
Antibiotics and Thromboprophylaxis: Post-operative antibiotics were administered for 24 hours to prevent infection. Thromboprophylaxis (e.g., low molecular weight heparin or direct oral anticoagulants) was initiated in all patients to reduce the risk of deep vein thrombosis (DVT), particularly in the early immobile phase.
Wound Care: Surgical wounds were monitored and dressings were done. Sutures/staples were removed after 12–14 days post-operatively, depending on wound healing.
Initial Mobilization: Passive range of motion exercises of the knee and ankle joints were started on post- operative day 1, under the guidance of a physiotherapist. Gentle quadriceps strengthening exercises were initiated early to prevent muscle atrophy and stiffness.
Weight-Bearing Protocol
The approach to weight-bearing was individualized for each patient but followed a general guideline for both the Suprapatellar and Infrapatellar groups.
1 month: All patients were restricted to partial weight-bearing during this period, using crutches or a walker. This restriction aimed to minimize stress on the healing tibia while encouraging early mobilization. Weight-bearing was limited to 20-30% of the patient’s body weight, allowing the fracture site to begin early biological healing without excess stress. Active range of motion exercises were advanced, including knee flexion-extension exercises to achieve 90 degrees of knee flexion by the end of week 6.
Week 6 to Week 12: Between 6 and 12 weeks, patients in both groups were transitioned to full weight-bearing as tolerated based on clinical and radiological signs of fracture healing.
Radiographs were taken at the 1-month mark to assess callus formation and fracture alignment. If satisfactory healing was observed, patients were encouraged to progress toward full weight-bearing by week 12. During this phase, strengthening exercises for the quadriceps, hamstrings and calf muscles were intensified and patients were encouraged to perform functional activities.
At 12- 18 weeks: Full weight-bearing without assistance should be achieved during this period, assuming good radiographic signs of fracture healing.
At 18- 24 weeks: Patients should be fully weight-bearing without assistive devices. By the end of 24 weeks, patients should be ready to resume most activities of daily living (ADLs), including walking, light jogging and non-impact sports.
Results
Functional Outcomes
Lysholm Knee Score
The Lysholm Knee Score was evaluated at 1 month, 3 months and 6 months post-operatively. The results showed that the Suprapatellar group had consistently higher scores, indicating better knee function compared to the Infrapatellar group, particularly at 3 and 6 months.
Table 1
Comparison of post-operative Lysholm Score between two groups
In 1 month, the suprapatellar group had a higher Lysholm score (68.8± 5.51) than the Infrapatellar group (65.35± 5.86), though the difference was not statistically significant (p = 0.063).At 3 months, the difference became significant, with the Suprapatellar group scoring higher (81.55± 4.54) than the Infrapatellar group (77.6± 6.29) (p= 0.028). At 6 months, the Suprapatellar group continued to outperform the Infrapatellar group, with a score of 92.2± 5.35 compared to 87.95± 5.34, a statistically significant difference (p = 0.016)(Table 1).This suggests that patients in the Suprapatellar group experienced faster and better functional recovery of the knee.
Lower Extremity Functional Scale (LEFS) Score
The LEFS score, which assesses the overall lower extremity function in daily activities, showed similar trends.
Table 2
Comparison of post-operative LEFS score between two groups
At 1st Month: The Suprapatellar group had a mean LEFS score of 68.80± 7.21, while the Infrapatellar group had a mean score of 64.65± 8.00. The difference was not statistically significant (p = 0.075), with a 95% confidence interval for the difference ranging from -0.55 to 8.02. This suggests a trend toward better function in the Suprapatellar group, but the difference is not significant at 1 month. By the third month, the Suprapatellar group had a significantly higher LEFS score (81.55± 5.69) than the Infrapatellar group (76.55± 5.77) with a p-value of 0.016. The confidence interval for the difference ranged from 1.04 to 9.46, indicating a significant functional advantage for the Suprapatellar group. At 6 months, the difference in LEFS scores remained significant. The Suprapatellar group scored 88.20± 4.54, while the Infrapatellar group scored 82.10± 5.86 (p= 0.025)(Table 2). The 95% confidence interval for the difference was 0.84 to 11.76, indicating a continued functional advantage for the Suprapatellar group.
Pain Outcomes
Visual Analog Scale (VAS) Score
Pain levels were measured using the VAS score at each follow-up point. The Suprapatellar group reported consistently lower pain levels compared to the Infrapatellar group.
Table 3
Comparison of post-operative VAS between two groups
At 1 month, the Suprapatellar group had a mean VAS score of (4.5± 0.50), compared to (5.0± 0.70) in the Infrapatellar group (p value= 0.020). Pain levels continued to decrease over time and at 3 months, the Suprapatellar group had a mean VAS score of (3.0± 0.40), while the Infrapatellar group had a mean score of ( 3.50± 0.60)(p-value= 0.003). By 6 months, the Suprapatellar group reported a mean VAS score of (2.0± 0.30), while the Infrapatellar group had a mean score of (2.50± 0.50)(Table 3). This reflects further pain improvement in both groups, with the Suprapatellar group showing lower pain levels and the p-value was 0.001, indicating a significant difference between the two groups, with the Suprapatellar group experiencing less pain. These findings indicate that patients in the Suprapatellar group experienced less post-operative pain throughout the recovery period.
Radiological Outcomes
Table 4
Comparison of post-operative radiological outcomes between two groups
At 1 Month: The Suprapatellar group had a mean alignment success rate of 95%, compared to 90% in the Infrapatellar group. At 1 month, the focus is primarily on maintaining proper alignment, as fracture union is not typically expected, With a t-value of 4.45 and a p-value of 0.0001, the groups' alignment success differed statistically significantly. It is anticipated that there will be some alignment and unification in three months. Mean alignment success rates for the Suprapatellar and Infrapatellar groups were 98% and 92%, respectively. Because of the non-union case and infection in this group, which affected the radiological results, there was a small decline in the Infrapatellar group. 6 months. The Infrapatellar group had 91% alignment success (Figure 5), while the Suprapatellar group achieved 99% Figure 8 . At every time point, the Suprapatellar group continuously showed better alignment outcomes, with a greater success rate and less variation in outcomes (Table 4).
Post-Operative Complications: Complications like infection and non-union affected the Infrapatellar group, which led to poorer alignment success results. This is in line with research showing that the Infrapatellar approach causes more anterior knee discomfort and problems because it irritates the patellar tendon and reduces fracture reduction precision. With just one instance of delayed union, the Suprapatellar group had better results and fewer problems.
Loss to Follow-Up: Even after taking into consideration the five patients who were not followed up at six months, the Suprapatellar group's results remained better. In terms of alignment and union rates, the Suprapatellar method is a more successful strategy, as evidenced by the statistically significant difference between the two groups.
Discussion
This study compared the functional and radiological results of intramedullary nailing procedures used to treat proximal tibia extra-articular fractures using suprapatellar (SPN) and infrapatellar (IPN) methods. Given its capacity to facilitate fracture healing by early mobilization, intramedullary nailing has emerged as the gold standard for treating proximal tibia fractures, which are among the most frequent long-bone fractures. However, because suprapatellar and infrapatellar techniques differ in surgical technique, complications and post-operative outcomes, the decision between them is still up for debate.
The average age of patients in the infrapatellar and suprapatellar groups is (37.5±14.89) years and (38.9±14.39) years, respectively. About 80% of patients in the suprapatellar group were men and 20% were women. Thirty percent of patients in the infrapatellar group were female and seventy percent were male.
According to this study, road traffic accidents (RTAs) were the most frequent cause of proximal tibia extra-articular fractures, accounting for 50% of cases in the suprapatellar group and 60% in the infrapatellar group. In total, motor accidents accounted for 55% of the fractures. The second most common cause, accounting for 25% of fractures in the suprapatellar group and 20% in the infrapatellar group, or 22.5% of all injuries, were falls from height. 15% of the cases in the Suprapatellar group and 10% in the Infrapatellar group, or 12.5% of the total, were related to sports injuries. Five percent of fractures in both groups were caused by direct strikes and working mishaps, but no other major injury cases were reported.
The Lysholm Knee Score, Lower Extremity Functional Scale (LEFS) and Visual Analog Scale for Pain (VAS) were used to assess the functional results in this study. In comparison to the Infrapatellar group (IPN), the Suprapatellar group (SPN) showed a statistically significant improvement in functional recovery at three and six months. Lysholm Knee Score, at 6 months suggests that the Suprapatellar group's mean score was (92.2±5.35), while the Infrapatellar group's was 87.95±5.34 (p = 0.016). This suggests that the SPN group recovered knee function more quickly. This discrepancy is probably because the SPN approach prevents irritation of the patellar tendon and extensor mechanism, which results in less soft tissue stress. According to research by Courtney et al.,(2015), suprapatellar nailing also improves knee function, especially in complicated fractures where correct alignment is essential.12
At three and six months, there was a notable functional improvement in the Suprapatellar group's LEFS scores. At six months, the IPN group's mean score was (82.10±5.86) (p = 0.025), whereas the SPN group's was (88.20±4.54). This result confirms past research, including the study of Yang et al., (2018), which showed that suprapatellar nailing facilitated a faster return to daily activities and an earlier onset of weight-bearing.13
The Suprapatellar group also performed better on the VAS, with much lower pain scores recorded at every time point. The mean VAS score at 6 months was (2.0±0.30) for the SPN group and (2.5±0.50) for the IPN group (p = 0.001). This is consistent with research by MM Rakesh et al. (2023), who found that the suprapatellar approach lessens anterior knee pain, which is a common side effect of infrapatellar nailing because of the way the patellar tendon is compressed during surgery.14
At six months, 91% of patients in the Infrapatellar group had achieved union, while 99% of patients in the Suprapatellar group had done so. The non-union case in the Infrapatellar group and the delayed union case in the Suprapatellar group demonstrate the difficulties in obtaining the best possible fracture healing with the infrapatellar approach. Proximal tibia fractures have been demonstrated to be better controlled using the suprapatellar method, which results in more precise fracture reduction and quicker healing. The Suprapatellar group had a greater alignment success rate at every time point, with 95% alignment success at one month and 100% at six months, as opposed to 90% and 95% for the Infrapatellar group, respectively. According to studies carried out by Courtney et al.,(2015) and Tejwani et al.,(2014), suprapatellar nailing reduces the incidence of malalignment by offering better control over both proximal and distal fractures.12, 15
The Infrapatellar group in this study experienced one case of infection, while the Suprapatellar group experienced one incidence of delayed union. In addition, the Infrapatellar group experienced one instance of non-union. The patient in the Infrapatellar group healed without any further difficulties after the infection case was treated with antibiotics and debridement. However, because the surgical entrance point and the patellar tendon are so close together, the infrapatellar technique is known to carry a risk of infection. Because the surgical entrance point is so close to the patellar tendon, MM Rakesh et al.,(2023) discovered that anterior knee discomfort and infection are more common with infrapatellar nailing. It emphasizes how the infrapatellar approach, especially when tendon irritation is present, is linked to an increased risk of soft tissue problems, such as infection and delayed healing.14 In 2019, Xu et al., revealed in a meta-analysis that, because of the anatomical difficulties with the patellar tendon, infrapatellar nailing was more likely to result in problems such as infection, delayed union and non-union.16
According to Wang et al.,(2018), the suprapatellar technique outperformed the infrapatellar method in terms of reduced fracture risk, improved knee functional recovery, decreased knee discomfort (as measured by a lower VAS pain score) and shorter fluoroscopy time.17
According to Gao et al., (2022),18 the group using the suprapatellar technique had a mean Lysholm score of 86.21 ± 10.75 points and a mean VAS score of 1.31 ± 0.43 points. The mean VAS score was 1.21 ± 0.38 points and the mean Lysholm score was 82.82 ± 10.62 points in the infrapatellar approach group. There was no significant difference in either of the parameters between the two groups (P= 0.070 and P= 0.161, respectively).9
Limitation
Small Sample Size: There were only 40 patients in the trial, 20 in each of the suprapatellar and infrapatellar groups. A limited sample size can raise the possibility of type II errors (failing to identify a difference when one exists) and limit how broadly the results can be applied. In order to draw more firm conclusions on the distinctions between these methods, larger studies would yield more reliable data.
Short Follow-Up Duration: This study's 6-month follow-up period could not have been enough to record long-term issues such as delayed union, non-union, late-onset infections and functional recovery over a longer time frame. More information about the durability and long-term effects of the suprapatellar and infrapatellar procedures would be available with longer follow-ups.
Conclusion
The purpose of this study was to compare the functional, radiological and results of infrapatellar (IPN) and suprapatellar (SPN) nailing methods for the treatment of proximal tibia extra-articular fractures. The Suprapatellar group showed a statistically significant advantage in the functional results of this trial, as determined by the Lysholm Knee Score, Lower Extremity Functional Scale (LEFS) and Visual Analog Scale (VAS) for pain. Patients who had suprapatellar nailing at three and six months demonstrated improved knee function, less pain and a speedier return to their regular activities. According to radiological evaluations, the Suprapatellar group outperformed the Infrapatellar group in terms of fracture alignment and union rates. At six months, the Suprapatellar group had a 100% alignment success rate, whereas the Infrapatellar group had a 95% success rate. This shows how well the suprapatellar approach controls fracture reduction. The Suprapatellar group also had higher union rates, with 99% of fractures mending after 6 months, as opposed to 91% in the Infrapatellar group. This discrepancy might result from the suprapatellar technique's improved capacity to preserve correct alignment, particularly in proximal tibia extra-articular fractures, where the infrapatellar approach is more likely to cause malalignment. It is well recognized that the risk of these problems is increased when the patellar tendon is close to the surgical entry point during infrapatellar nailing. Because of the nature of the procedure, this result is consistent with other research that showed a link between infrapatellar nailing and soft tissue problems.