- Visibility 237 Views
- Downloads 37 Downloads
- Permissions
- DOI 10.18231/j.ijos.2024.065
-
CrossMark
- Citation
Revision capitellum fracture fixation: A surgical challenge case report
Abstract
Capitellum fractures are rare, accounting for 1% of all elbow fractures and pose a unique challenge due to their intra-articular nature and susceptibility to displacement. This case report details a revision surgery for a 31-year-old male who sustained a displaced intra-articular capitellum fracture following a fall. Initial treatment with open reduction and internal fixation (ORIF) using two Herbert Headless Compression Screws failed due to inadequate reduction and early mobilization, resulting in non-union and persistent pain. A revision surgery was performed using three herbert screws, achieving successful reduction and fixation. Postoperative rehabilitation led to a significant improvement in elbow range of motion and function over 11 years of follow-up. This report emphasizes the importance of careful surgical planning, preservation of vascularity, appropriate fixation techniques and adherence to rehabilitation protocols to prevent complications and ensure favorable outcomes in revision capitellum fracture surgeries.
Introduction
The capitellum forms a component of the distal most part of the lateral column of the articulating surface of the humerus. Isolated fractures of the capitellum represent 1% of all elbow fractures and 6% of distal humeral fractures.[1] They occur most commonly in the coronal plane, parallel to the anterior humerus. Due to the paucity of attachments to the capitellum, a fracture results in a free articular fragment that may displace. The mostly cartilaginous composition of the capitellum below 10 years of age makes it more resistant to stress. As the capitellum grows and ossifies in older children, it becomes more susceptible to a shear injury. A capitellum fracture is an intra-articular osteochondral fracture.[1] The most common mechanism of injury in a capitellum fracture is a fall onto an outstretched hand with the elbow in varying degrees of flexion. This causes the force to be transmitted via the radial head to the capitellum resulting in a shear force leading to a fracture.[2] The capitellum is particularly susceptible to shear forces as its centre of rotation is more anterior to the humeral shaft.[1] The currently accepted classification of capitellum fractures includes Type I Hahn-Steinthal fragment which comprises of a large osseous fragment of the capitellum which may involve part of the trochlea. Type II is a Kocher Lorenz fragment with an articular cartilage with minimal subchondral bone attached also called as an uncapping of the condyle. Type III was described by Morrey which is a markedly comminuted fracture. McKee et al described Type IV which is a shear fracture of the capitellum in the coronal plane extending into the trochlea. According to the OTA classification, an isolated capitellum fracture is classified as 13B3.13. An isolated fracture of the capitellum in itself is a rarity which is not described in many studies. Treatment involves fixation or excision. There have been reports of good functional outcomes following excision of fracture fragments as well.[3] In this case report we shall be delving into a revision surgery of a capitellum fracture and the outcome and treatment protocol associated with it.
Case Presentation
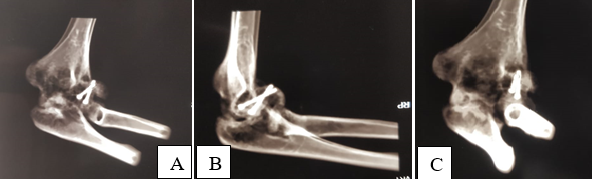
A 31-year-old male had a history of fall on black ice while skiing with axial loading extension type injury through the radial head to the left (non dominant) hand on 30/01/2011 in New Jersey, USA. On initial evaluation and radiographs the patient was diagnosed to be having a displaced intra-articular fracture of the capitellum. On examination, there was bruising and local tenderness over the capitellum along with crepitus and reduced range of motion. The three-point bony relationship was maintained ([Figure 1], [Figure 2], [Figure 3]).
The patient was taken up for his initial surgery on 15/02/2011 in New Jersey, USA with a standard lateral approach to the capitellum and the fracture was fixed with Open Reduction Internal Fixation with two Herbert Headless Compression Screws ([Figure 4]).
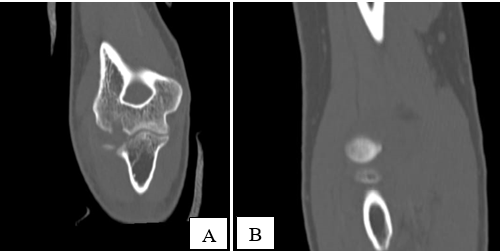
Postoperatively, the patient started experiencing pain at the fracture site after range of motion exercises were started with a hinged elbow brace on postoperative day two. There was severe restriction of ROM and persistent pain due to which the patient was unable to adhere to the physiotherapy protocols. He followed up with the operating orthopaedician five weeks postoperatively for persistent disability and a fresh CT scan was done on 22/03/2011 which showed a displaced capitellum with the implants in situ. Patient was advised to start a trial of physiotherapy by the operating Orthopaedician after examining the CT scan. The patient underwent a trial of physiotherapy for another four weeks without any relief in his symptoms after which he was advised to undergo a revision surgery to fix the Capitellum again in May 2011 ([Figure 5]).
The patient then came to India in the first week of June 2011 with complains of persistent pain, stiffness and crepitus at the elbow along with restricted range of motion which hampered his daily activities. On the 5th of June, 2011 when he first presented to our centre, he had tenderness over the Capitellum, elbow range of motion 30-70 degrees along with stiffness in the midprone position ([Figure 6], [Figure 7], [Figure 8]).
He was operated for a revision ORIF on 08/06/2011 with fixation of the displaced capitellum fragment with three Herbert screws after removing the two Herbert screws that were previously holding the fracture. Postoperatively the patient was put in an above elbow slab for four weeks followed by gradual non loading range of motion exercises ([Figure 9], [Figure 10]).
During his 11 year follow up postoperatively after the second procedure, the patient had left elbow ROM as follows:
Flexion- 5 to 150 degrees
Pronation- 90 degrees
Supination upto 85 degrees.
The patient now has no pain over the elbow and can manage his daily activities ([Figure 11], [Figure 12], [Figure 13], [Figure 14], [Figure 15]).













Discussion
An isolated fracture of the capitellum is often missed due to bad radiological examinations as well as due to inexperience in the interpretation of an elbow x ray. Capitellum fractures however, have a significant disability with restriction of elbow movements which will lead to stiffness if not treated at the right time. Leaving it untreated, causes elbow stiffness and limitation of elbow movements and if excised, can cause instability of the elbow. Hence it is pivotal to not only reduce the fracture of a capitellum adequately but also to ensure that the elbow rehabilitation is early so as to prevent any stiffness in an adequately reduced fracture. In cases with isolated noncomminuted capitellar and/or trochlear fractures, the outcome is better compared to more complex cases.[4]
MD McKee et al, described a characteristic radiological abnormality, described as the ‘Double arc sign’, seen on the lateral radiograph in which the subchondral bone of the displaced capitellum overlaps with the lateral trochlear ridge.[5]
There are various modalities for treatment of a capitellum fracture via open reduction and fixation with K wires or Herbert Headless Compression screws. A study carried by Poynton et al. suggested that fixation of a displaced intra-articular fracture of the capitellum is best fixed with a Herbert headless compression screw as it allows for early post op mobilization and better functional outcome.[6]
The choice of treatment depends on various factors like age, character of the bone and the type of fracture.[7] In this particular case, the patient had been operated with two Herbert Headless compression screws during primary fixation. Due to inadequacy in the reduction as well as early post op mobilization, the fracture failed to unite.
During the revision surgery, the most important factors to be considered were the displacement of the fracture fragments, preserving the vascularity of the fracture fragment, direction of the screws, the approach and the post op rehabilitation protocol.
The fracture on presentation had a fragment which had displaced anteriorly and laterally with intra-articular extension. To reduce this fracture, the patient had a primary surgery with fixation using two AO type screws in the postero-anterior direction which did not adequately reduce the displacement in the coronal plane. Hence when the patient was mobilized on post-operative day two it caused displacement of the inadequately reduced fracture and thus caused pain and stiffness of elbow movements to the patient.
In order to reduce an intra-articular fracture with restoration of articular surface congruity, it requires early anatomical reconstruction, stable fixation with interfragmentary compression and early motion in adherence to AO principles of articular fracture fixation.[8] Keeping these principles in mind, our goal was to not only reduce the fracture adequately but also to ensure that with the correct post-operative rehabilitation protocol the patient does not suffer from stiffness of elbow movements later.
Apart from adequate reduction, the vascularity of the displaced fracture fragment had to be taken into consideration to ensure bony union. The capitellum and the lateral aspect of the trochlea are supplied by the posterior perforating vessels arising from the radial recurrent, radial collateral and interosseous recurrent arteries. Preserving this vasculature during revision surgery was pertinent to bony union.[9]
During the revision surgery, the patient was operated using the previous incision. The first step of the revision surgery entailed removing the two Herbert Headless compression screws (3.5mm) used during primary fixation. After removal of the two screws, allograft bone was inserted into the fracture site, the fracture was reduced and the reduction was held in place with the help of K wires provisionally. The three Herbert Headless compression screws were then threaded over the K wires and the K wires were then removed. The fracture fragment was held in place using three screws in AP direction in a diverging fashion. Alternatively, one can also use fully threaded Headless compression screws for a similar result.[10] Postoperatively the patient was put in an above elbow slab for four weeks followed by early range of motion exercises of the elbow after four weeks of immobilization in slab. The result was such that the patient developed near complete range of motion of the elbow with gradual and consistent physiotherapy.
Conclusion
A revision capitellum surgery albeit challenging considering the difficulty in reduction and the proximity to various neurovascular structures is not a difficult task if tackled with careful pre-operative planning and assessment of the patient.
Intra-operatively, the surgeon should be careful to not mishandle or devascularize the fragment. Once reduced, the fracture should be fixed with Herbert Headless compression screws preferably from anterior to posterior direction which is stronger biomechanically.
In revision scenarios, at least three to four headless compression screws should be used for better torsional control.
Postoperatively, the patient should be kept in an above elbow slab for two weeks in order to allow for soft tissue healing and pain control followed by hinge elbow ROM bracing. The functional outcome score in this case was 30/100 pre operatively according to ASES score which improved to 97/100 on an 11 year follow up.[11]
Patient Consent
Author consent was taken prior to publication.
Conflicts of Interest
None.
Source of Funding
None.
References
- Kalawar R, Chaudhary P, Maharjan R, Afaque S. An isolated capitellum fracture of the humerus in adult: A rare case report. Health Renaissance. 2015;13(1):112-6. [Google Scholar]
- Egol K, Koval K, Zuckerman J. . Handbook of Fractures. 2019. [Google Scholar]
- Alvarez E, Patel M, Nimberg G, Pearlman H. Fractures of the capitulum humeri. J Bone Joint Surg Am. 1975;57(8):1093-6. [Google Scholar]
- Dubberley J, Faber K, Macdermid J, Patterson S, King G. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am. 2006;88(1):46-54. [Google Scholar]
- Mckee M, Jupiter J, Bamberger H. Coronal shear fractures of the distal end of the humerus. J Bone Joint Surg Am. 1996;78(1):49-54. [Google Scholar]
- Poynton A, Kelly I, O'Rourke S. Fractures of the capitellum-a comparison of two fixation methods. Injury. 1998;29(5):341-3. [Google Scholar]
- Grantham S, Norris T, Bush D. Isolated fracture of the humeral capitellum. Clin Orthop Relat Res. 1981;161:262-9. [Google Scholar]
- Ruchelsman D, Tejwani N, Kwon Y, Egol K. Open reduction and internal fixation of capitellar fractures with headless screws. J Bone Join Surg Am. 2008;90(2):38-49. [Google Scholar]
- Yamaguchi K, Sweet F, Bindra R, Morrey B, Gelberman R. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am. 1997;79(11):1653-62. [Google Scholar]
- Pogliacomi F, Concari G, Vaienti E. Hahn-Steinthal fracture: report of two cases. Acta Biomed. 2005;76(3):178-84. [Google Scholar]
- Lamplot J, Lillegraven O, Brophy R. Outcomes from conservative treatment of shoulder idiopathic adhesive capsulitis and factors associated with developing contralateral disease. Orthop J Sports Med. 2018;6(7). [Google Scholar]
How to Cite This Article
Vancouver
Kulkarni S, Malnas M, Rao A, Munshi P. Revision capitellum fracture fixation: A surgical challenge case report [Internet]. Indian J Orthop Surg. 2024 [cited 2025 Sep 17];10(4):395-400. Available from: https://doi.org/10.18231/j.ijos.2024.065
APA
Kulkarni, S., Malnas, M., Rao, A., Munshi, P. (2024). Revision capitellum fracture fixation: A surgical challenge case report. Indian J Orthop Surg, 10(4), 395-400. https://doi.org/10.18231/j.ijos.2024.065
MLA
Kulkarni, Shradha, Malnas, Mansoor, Rao, Aditya, Munshi, Parag. "Revision capitellum fracture fixation: A surgical challenge case report." Indian J Orthop Surg, vol. 10, no. 4, 2024, pp. 395-400. https://doi.org/10.18231/j.ijos.2024.065
Chicago
Kulkarni, S., Malnas, M., Rao, A., Munshi, P.. "Revision capitellum fracture fixation: A surgical challenge case report." Indian J Orthop Surg 10, no. 4 (2024): 395-400. https://doi.org/10.18231/j.ijos.2024.065
