Introduction
Femoral head fracture is an unusual injury induced by high velocity trauma that is most commonly associated with traumatic posterior dislocation of the hip. Late diagnosis inevitably leads to poor prospects and beyond repair difficulties, which may subsequently require hip joint surgery.1 The femoral head fracture was first reported by Birkett, in1869.2 Pipkin subsequently presented an assessment scheme for femoral head fractures in 1957.3 He categorized into four types. Type I includes fracture inferior to the fovea. Type II includes fracture superior to the fovea. Type III includes type I and II fracture associated with femoral neck fracture. Type IV includes type I and II fracture associated with acetabular fracture. Numerous surgical alternatives have been documented to manage the femoral head fracture, however they have been linked with a significant complication rate. 4, 5, 6, 7, 8 They do, however, restrict complete access to the femoral head. This difficulty is avoided by Ganz safe surgical hip dislocation, which also has the benefit of protecting and preserving the femoral head's blood flow.
When fixing femur head fractures, the Kocher-Langenbeck and Smith-Petersen anterior approaches are the two approaches that are commonly used.4, 5 For the treatment of traumatic hip joint injuries, the controlled hip dislocation technique emerged. The technique was first described by Reinhold Ganz for the open treatment of femoroacetabular trauma in the early 1990s. It enables the immediate reduction of fragments and their securement with suitable implants, as well as the visualization of the entire circumference of the femoral head with minimal risks of arterial supply damage. The procedure involves controlled anterior hip dislocation of the femoral head and greater trochanter osteotomy.9 In his case series, Reinhold Ganz failed to report any osteonecrosis cases.10 In this case presentation, we describe a patient who had treatment using the Ganz safe surgical hip dislocation technique and the modified Gibson approach after suffering a Pipkin Type-II posterior fracture dislocation of the femoral head as a result of high intensity trauma.
Case Presentation
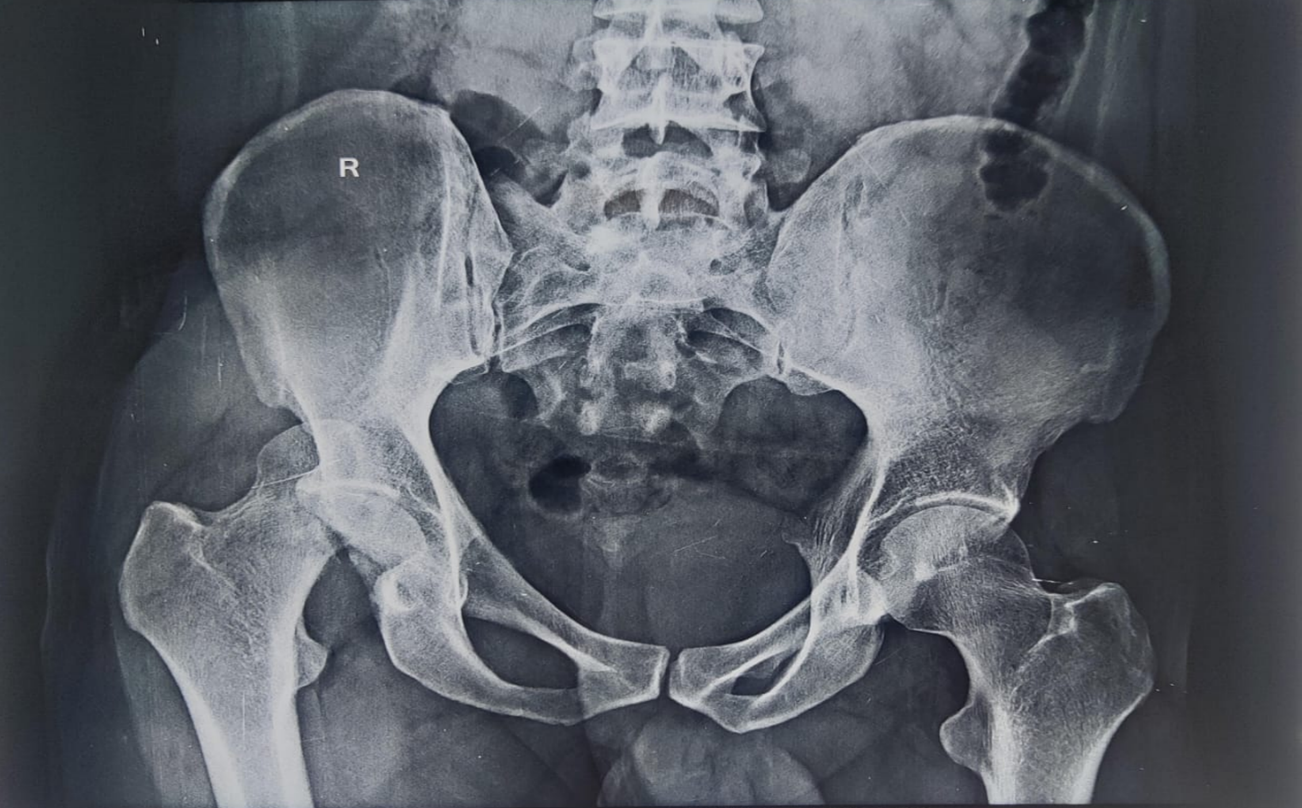
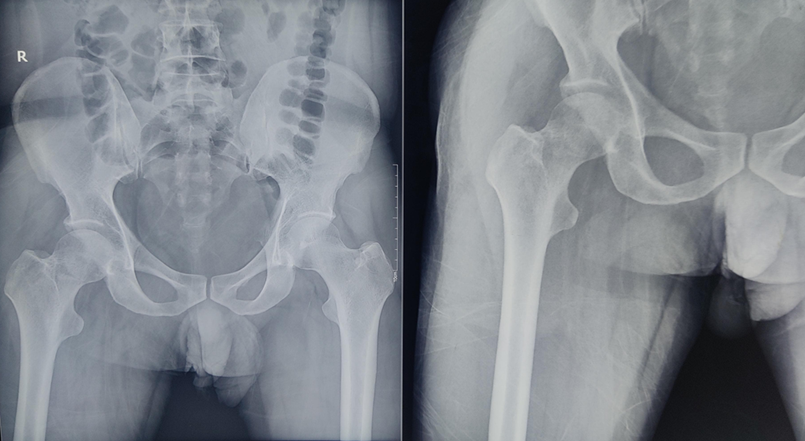
A 33 years old male patient presented to the emergency department at MMIMSR with an alleged history of a motor vehicle collision, following which he complains of pain deformity over right hip region. On evaluation, his right lower limb was flexed, adducted and internally rotated and limb was shortened. Upon radiological investigation, posterior hip dislocation was found (Figure 1), it was effectively reduced by the Allis procedure for close correction of posterior hip dislocation.11 Hip was repeatedly dislocated; after several efforts, the hip was repositioned and stabilized by skin traction in its anatomical place. Adequate X-rays confirmed the relocation (Figure 2). The patient had C.T. pelvis with multiplanar and 3D reconstruction, which suggested a Pipkin type II femoral head fracture on the right side (Figure 3).
The patient achieved femoral head fixation with numerous Herbert screws via a modified Gibson approach 12 and the Ganz safe surgical hip dislocation and trochanteric flip osteotomy procedure. 10 During the surgical procedure, the patient was positioned in the lateral decubitus position and a longitudinal incision was made from the iliac crest, continuing over the greater trochanter and down the lateral thigh.
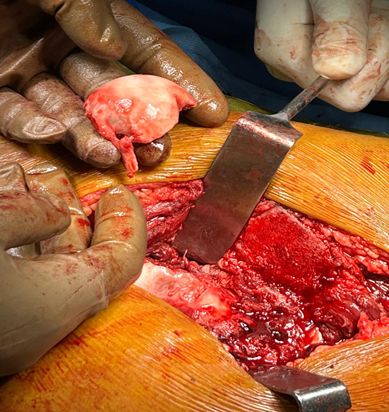
After deep dissection, the greater trochanter was osteotomized and a 1.5mm thick osteotomized greater trochanteric flap was raised (Figure 4) following that, the short external rotators were spotted; in our case, all of the short external rotators had been ruptured (Figure 5). Except piriformis, which was entire, no discontinuity in the fibers of piriformis was noticed.
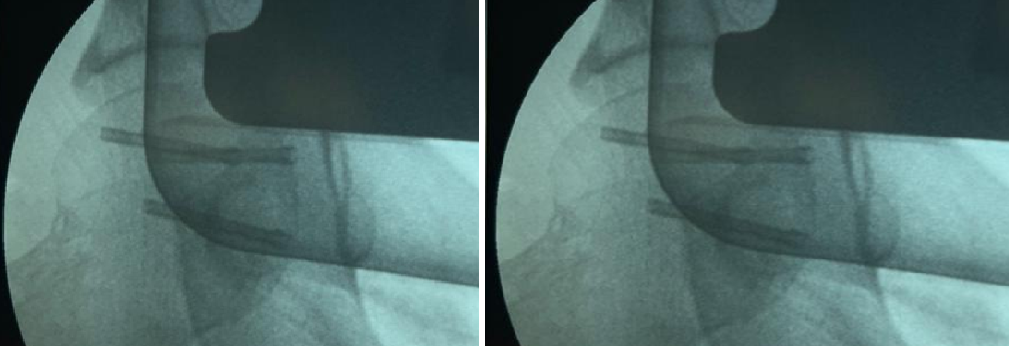
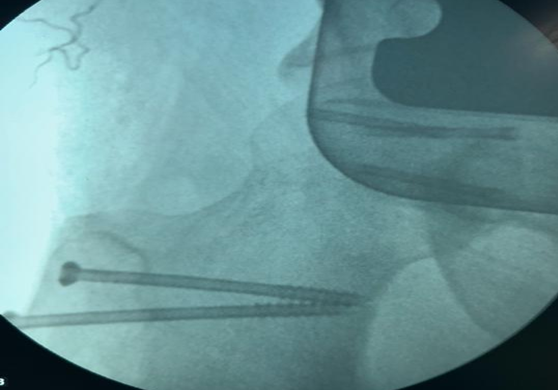
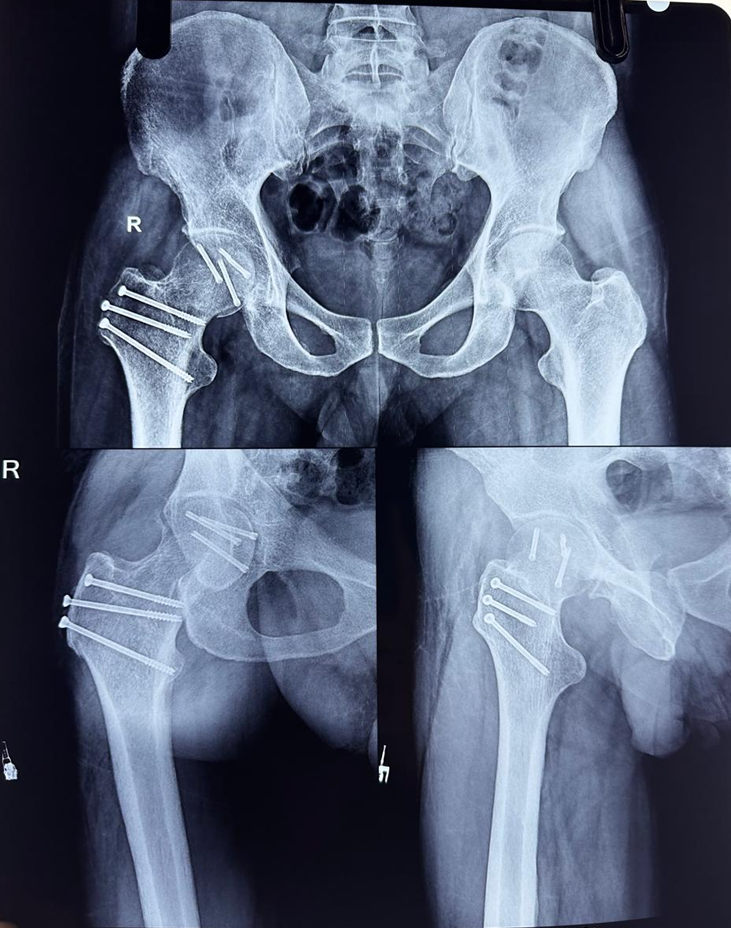
The femoral head fracture was exposed (Figure 6) and femoral head was fixed with 3mm Herbert screws (Figure 7). After validating the vascularity of the femoral head, by executing the drilling test. The screws' reduction and integrity were verified using a C-arm. Three 6 mm screws were used to secure the greater trochanter flap following the repair of broken short external rotators were fixed (Figure 8).
Postoperatively, X-rays were taken (Figure 9), no complications were seen and toe weight bearing walker aided mobilization was performed.
At the 6-months follow up, the patient is mobilizing full weight bearing without complaining of pain and there was no evidence of avascular necrosis on the x-ray (Figure 10).
Discussion
The combination of posterior hip dislocation and femoral head fracture is generally the result of a high velocity injury, particularly a dashboard injury in a motor vehicle collision. The posterior hip dislocation and femoral head fracture occur in 4-17% of patients.6 Immediate close reduction in an emergency is encouraged in order to avoid femoral head avascular necrosis.13 Conservative treatment might be considered as an option for un-displaced fracture, but problems associated to protracted immobility time period are encountered in such individuals.
Although several surgical procedures are available, there is continuous discussion on which approach yields the greatest results and has fewer complications. For such cases, a controlled surgical hip dislocation technique has recently been implemented; it provides better visibility and the chance to detect and ultimately cure labral tears or posterior wall abnormalities. According to Mostafa et al., surgical hip dislocation with trochanteric osteotomy led to less blood loss and a quicker recovery period. Due to benefits including direct screw fixation, full exposure of the femoral head and a decreased risk of osteonecrosis, he concluded that the surgical hip dislocation procedure was superior to the posterior approach.4
Letournel and Judet's Kocher-Langenbeck posterior approach gives access to the acetabulum's posterior wall and posterior column. By moving the superior limb of the incision further anteriorly, Gibson enhanced this technique. Moed went on to explain a variation of the Gibson technique that preserves the neurovascular supply to the anterior part of the gluteus maximus muscle by making a straight lateral incision. Additionally, this technique permits the acetabulum and iliac wing to be exposed to the anterior portion of the body to a greater extent.12
The Ganz safe surgical hip dislocation technique was initially described as an open therapy for femoroacetabular impact. The Ganz technique has just recently acquired popularity; it serves as a substitute to conventional approaches in such fractures.
Several authors describe the use of Herbert screws,4, 6, 14 partial cancellous screws,4, 14 headless screws,15 and non-absorbable screws5 as fixing methods for femoral head fractures. In the presentation mentioned above, Herbert screws were utilized. According to certain writers, compression is necessary for head fragment fixation in order to either embed head pieces together and prevent displacement or speed up the healing process.16 One rare intra-capsular injury in posterior wall acetabular fractures is a posterior labral rupture. 15 Since other authors have noted that an avulsed posterior root of the labrum is a sign that repair is necessary, a posterior labral tear was visible in our case and was sutured. It could impair the normal labrum's capacity to seal joints, leading the hip joint to be unstable. 15
According to published reports, the prevalence of osteonecrosis in cases of severe hip dislocation ranges from 8 to 24 percent. 4, 5, 13 Blood supply damage is the primary underlying cause of femoral head osteonecrosis and can happen during surgery or following a traumatic hip dislocation. Therefore, a crucial part of the surgical procedure is the intraoperative assessment of the vascularity of the femoral head utilizing the drilling technique. Additionally, for a favorable outcome and to prevent osteonecrosis, the interval between the hip dislocation injury and femoral head reduction is crucial.17, 18 In our case the close relocation of hip was achieved within 6 hours and drilling test was performed intra-operatively and vascularity of the femoral head was intact.
After a trochanteric flip osteotomy, the mean incidence of osteonecrosis is 12.5%; the anterior technique has an incidence of 7.9%, while the posterior hip approach has an incidence of 16.4%. The anterior hip approach had the highest prevalence of heterotopic ossification and a lesser frequency of osteonecrosis.19 Surgical hip dislocation improves visibility and makes it possible to identify and treat labral tears or disorders of the posterior wall.
One of the most reliable measures of femoral head longevity in patients undergoing surgery for hip dislocation is the drilling test, additionally referred to as the bleeding sign. When predicting femoral head vitality during surgical hip dislocation, Aprato et al. showed that the drilling test exhibited an 83% specificity and a 97% sensitivity.20 The longevity of the femoral head can be assessed intraoperatively. A negative drilling test indicates a higher risk of osteonecrosis and impoverished vascularity.
Although there is ongoing debate on the best surgical method for treating femoral head fractures, there is growing evidence in the literature that the Ganz procedure is both practical and advantageous.