Introduction
The femur plays a vital role in weight bearing in the lower extremities. The incidence of femur shaft fractures is 10 to 37 per 100,000 patients annually, with a peak in young men at age 27 years and in older women at age 80 years.1 High energy forces such as those that occur in car accidents and falling are common causes of femur shaft fracture. The common classification system for femur shaft fracture is the AO-Müller/Orthopaedic Trauma Association (AO/OTA) system, which includes the classification of all long bone fractures and femur shafts (diaphyseal), with fracture patterns mainly divided into three types: simple, wedge and complex fractures.2 Intramedullary nailing (IMN) is the preferred choice for treating femur shaft fracture with lesser complications (4.9%)3 still non union occurs in some cases. Open fracture, tobacco intake, delayed weight bearing, communited fracture, inadequate fracture reduction, may intervene in fracture healing and act as risk factors for non union.
Case Report
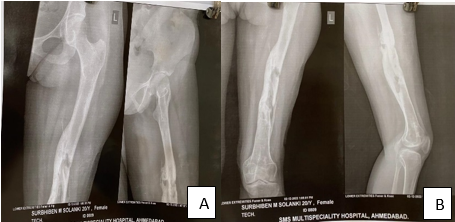
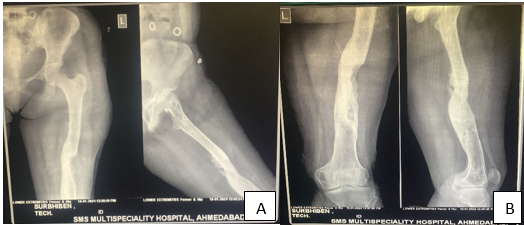
We report a case of 20 year female presented with left side infected non united shaft femur fracture with discharging sinus and history of femur interlocking nail followed by debridement and removal of implant.
The patient presented to our OPD with complaint of Pain over Left thigh and inability to walk with discharging sinus over Lateral aspect of thigh with purulent discharge (Figure 1-12).
Her Blood investigation were suggestive of High ESR, CRP Levels. X-Ray showed non-union of left side shaft femur fracture with osteomyelitic changes. The patient had history of road traffic accident and suffered multiple injuries with head injury and both side shaft femur fracture four years ago in 2020, following which patient underwent intramedullary nailing of both side shaft femur.
However on follow up left side shaft femur fracture remained non united with discharge present from proximal suture site.
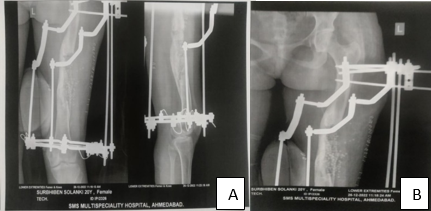
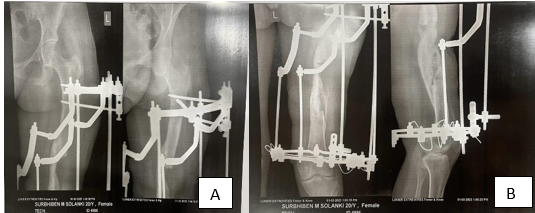
The patient then underwent 3 Stage Procedure of Debridement in 2021 followed by Debridement & removal of implant in march 2022 Followed by Debridement and Sequestrectory with Partial corticotomy with Stimulants insertion and Ilizarov fixation in December 2022.
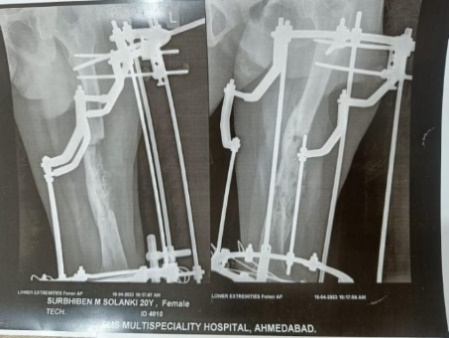
This was followed by Removal of Implant [Ilizarov ring] after 8 months in august 2023.
Post-operative care
Post op dressing was done on postoperative day 2 and day 5. Few sutures taken earlier were removed on post op day 14. The patient was made to walk and started with partial weight bearing with walker for 15-20 days then started with full weight bearing after a month of operation.
Subsequent ESR and CRP levels were done to check prognosis after 1 month post operatively and showed decreasing trends.
Result
The functional outcome of ilizarov fixation with seqestractomy and stimulant insertion was satisfactory. Patient was able to mobilise well. Bony union was achieved without any signs of infection. Patient is able to resume all her previous works with moderate level of ease. Initally variable oedma was present and persisted but disappeared soon after removal of frame. Patient was restless throughout the treatment course and given psychotherapy but recovered soon after being able to stand and walk. No neurovascular complications observed.
Discussion
Because of high velocity trauma, delayed presentation, infection of the soft tissues and bones, nonunion, bone loss, osteoporosis, dystrophy, poor vascularity, related deformities and shortening, the results of traditional treatment for infected nonunion of the femur are inadequate. In certain situations, the Ilizarov procedure produces good results. Gradual strain on living tissues, in Ilizarov's view, produces stress that both initiates and sustains tissue regeneration and active growth (bone, muscle, fascia, tendon, nerve, arteries, skin and its appendages). "The law of tension stress" is the name given to this idea.2 While improving the vascularity of the osteomyelitic center by biological stimulation of a corticotomy (osteomyelitis burns in the fire of regeneration) was the main goal of the Ilizarov treatment, infection was not always treated.
Consequently, it is advised to do a thorough debridement prior to distraction osteogenesis. Distraction osteogenesis is the process of mechanically stimulating the production of new bone between gradually separating bony surfaces. Bone transfer guarantees the movement of living bone segments to fill an intercalary bone defect following corticotomy. Through intramembranous ossification, the following end regenerates bone, while the leading end fused with the target bone surface.4 The degree of injury at the moment of corticotomy, the pace and rhythm of distraction and the rigidity of bone fragment fixation all affect the quantity and quality of osteogenesis that occurs during distraction.5 Since general body anabolism is an intrinsic biological response of the tissues to distraction, it should constantly be positively maintained.6 An inadvertent gap is made following sequestrectomy in cases of infected nonunion. Because of this non-union gap, external fixation is the best option because internal fixation is ruled out. There have been prior reports on the use of external fixation to treat infected nonunion of the femur.4 To close the gap left by the universal-type external fixation, multiple bone grafts must be made. Because of its cantilever fixation, mobilization is not possible due to insufficient mechanical strength. Larger pin-track issues are typical, as are disuse osteoporosis and refracture. Furthermore, its ability to rectify deformity and shortening is restricted. All these challenges can be overcome by the Ilizarov procedure. The Ilizarov frame build has a high mechanical resistance to bending and torsion, yet it permits axial compression under physiological loads.4 Ilizarov employed thin, tensioned wires, which take up less room and cause fewer pin-track issues.
However, placing wires in the proximal regions of the femur is challenging, less well tolerated and frequently fraught with consequences. As a result, ASAMI7 changed the frame and used a proximal half pin apparatus rather than a circular frame to get better overall outcomes. For the proximal femur, we employed a similarly adapted frame with Schanz screws through the arch. On the level of complete rings along the femur, the transfixation tensioned olive wires for the intermediate and distal rings are positioned in accordance with the goniometric atlas' instructions. Following the safe corridors of the proximal femur as outlined by ASAMI, the Schanz screws through the proximal arch are inserted in the trochanteric and subtrochanteric region.
This means that, in all practicality, pin insertion should begin from the lateral aspect of the trochanter and subtrochanteric region rather than the anteromedial and posteromedial regions of the proximal femur. The number of rings and the diameter, number, tension, degree of crossing and position of the wires along the bone's longitudinal axis all affect how stable an assembly is. Uniplannar half pin systems are vulnerable to cantilever loading, which causes the osteogenic site to become angularly unstable. Consequently, a multiplanar configuration is required when utilizing a half pin assembly in the proximal femur. Even while the biomechanics may not be as robust as the original Ilizarov apparatus's, it nonetheless accomplishes the same goal and is more easily tolerated and causes fewer issues.
It is a hybrid fixator that incorporates the ideas of two external fixation systems (proximal Schanz screws and distal tensioned wires), departing from the original Ilizarov concept of transfixing wires for the proximal femur.2 There was no use of the external tubular system. The amount and quality of regeneration are determined by the initial damage inflicted at the corticotomy site; therefore, during the procedure, it is important to minimize damage to the periosteal soft tissues, the nutrient artery and its branches and the bone marrow. The interval of time between a corticotomy and the start of a distraction is known as latency. While longer latency allows for early consolidation and fusion, shorter latency results in poor regeneration. It is advised to wait between 0 and 14 days following a corticotomy, depending on the extent of damage.
Physiological bone loading and mobilization are crucial during distraction osteogenesis. As soon as possible, the patient was placed on weight bearing and the physical therapist actively participated in joint mobilization. The distraction rate and rhythm were maintained at 0.25 mm/6 hours (1 mm/day) and are expected to stay between 0.5 and 2 mm/day. It may be necessary to use an intramedullary thin central guide wire and keep it in place until the moving bone segments reach the target site and the target nonunion site forms callus in order to improve assembly stability during bifocal osteosynthesis and lower the possibility of bone fragment displacement during transport. Axial deviation from larger gap regenerations may occur, requiring apparatus adjustment.The mean healing index of 38days/cm (standard deviation 1.6 days/cm) was similar to other reports on femur nonunion and limb lengthening. At the docking site, cancelous bone grafting or bone end refreshing may be necessary. Refreshing and cancelous bone grafting may shorten the frame-keeping time and speed up healing. Union was accomplished and infection was eradicated. Although difficulties are a natural part of the Ilizarov technique, they become less frequent and less severe with practice. Consistent with previous reports, the bone result was consistently superior to the functional result. The majority of patients arrive late, having already undergone several operations with significant damage to muscles, joints, bones, vessels and nerves, having already experienced varying degrees of joint stiffness. Over an intramedullary nail, bone transport provides extra stability and sortensh the duration of external fixation and its associated complications. However, it impairs endosteal circulation and is not suitable for insertion when an infection is active. It also increases the risk of necrosis of the moving segment and infection recurrence. To prevent vascular failure following vascularized fibular grafting, close observation of the blood supply and prompt intervention are necessary. Internal bone transport necessitates frequent debridements, bone grafting at the docking site for early union and stress fracture prevention in order to improve outcomes.8 The techniques of multiple segment lengthening, automatic high frequency lengthening and extemporaneous compression at the end of traction can significantly reduce the length of external fixation and any related complications.
Conclusion
Modified ilizarov technique is good salvage operation for infected non union of the femur. The bone results are usually superior to the functional result. Function results can be improved by early use of ilizarov technique. Limb salvage is always preferable to a prosthesis, So long as the limb is viable, adequately innervated and the patient is commited to the financial and psychological demands of the procedure.